- Audible rattling sounds or visible secretions in the tube
- Decreased breath sounds on chest auscultation
- Increasing respiratory effort or distress
- Suspicion of blocked or partially blocked tracheostomy tube
- patient requests suction
Consider suction prior to tracheostomy tube change, tape change, feeding, speaking valve use or after vomiting
- Only remove devices as required to pass a suction catheter (e.g. a cap, cover, speaking valve, HME filter and the inner tube of a dual lumen tube if it is present). Other devices such as the outer tracheostomy tube or laryngectomy tube (if present) should not be removed at this stage. Do not attempt to remove tracheoesophageal puncture valves / voice prosthesis embedded in the posterior tracheal wall.
- Pre-oxygenate the patient prior to aspirating the tracheostomy, and continuously monitor the patient’s condition.
When performing suction
- Ensure the patient is connected to a cardiac monitor and SpO2 probe when aspirating.
- Do not suction for more than 10 seconds in duration.
- It is not necessary to rotate the catheter as the multiple eyelet catheters will remove secretions effectively.
- To reduce the risk of infection:
- Protect the catheter tip from contamination before and in between passes. Do not allow to come into contact with surfaces, hands and clothing – discard if contaminated and use a new catheter.
- Whilst single-use suction tubing is preferable, provided no contamination to the suction catheter has occurred, it can be reused for multiple passes then discarded.
- If required, the tubing can be cleared by suctioning tap water through the suction tubing to clear it of secretions.
Preparing for and performing suction
- Position the patient, allowing access to the tracheostomy tube
- Attach the suction catheter to suction tubing, remove packaging and turn on the suction
- Insert catheter into tracheostomy tube to a maximum length of 15cm. If the patient is paediatric, please consult with carer or follow instructions on the patients Airway Profile for suction depth.
- If the catheter does not pass easily into the tracheostomy tube, do not force - suspect a blocked or partially obstructed tube.
- Suction should be applied on withdrawal of the suction catheter to minimise mucosal damage in the respiratory tract.
For general instructions, see Clinical Skill – Suction.
For further information, see article Tracheostomy in the Medical Library.
- Assess the patient and the effectiveness of secretion clearance. Repeat as necessary.
- Observe the patient during the procedure for signs of respiratory and cardiovascular instability and discomfort.
- Frequent repeat suctioning may be required if there are copious secretions.
- Consider other causes for respiratory distress if the stoma/tube is patent.
- If the patient improves following the removal of a blocked inner tube, it can be flushed with normal saline and reinserted if required (e.g. to facilitate reattaching the patient to a ventilator or a BVM).
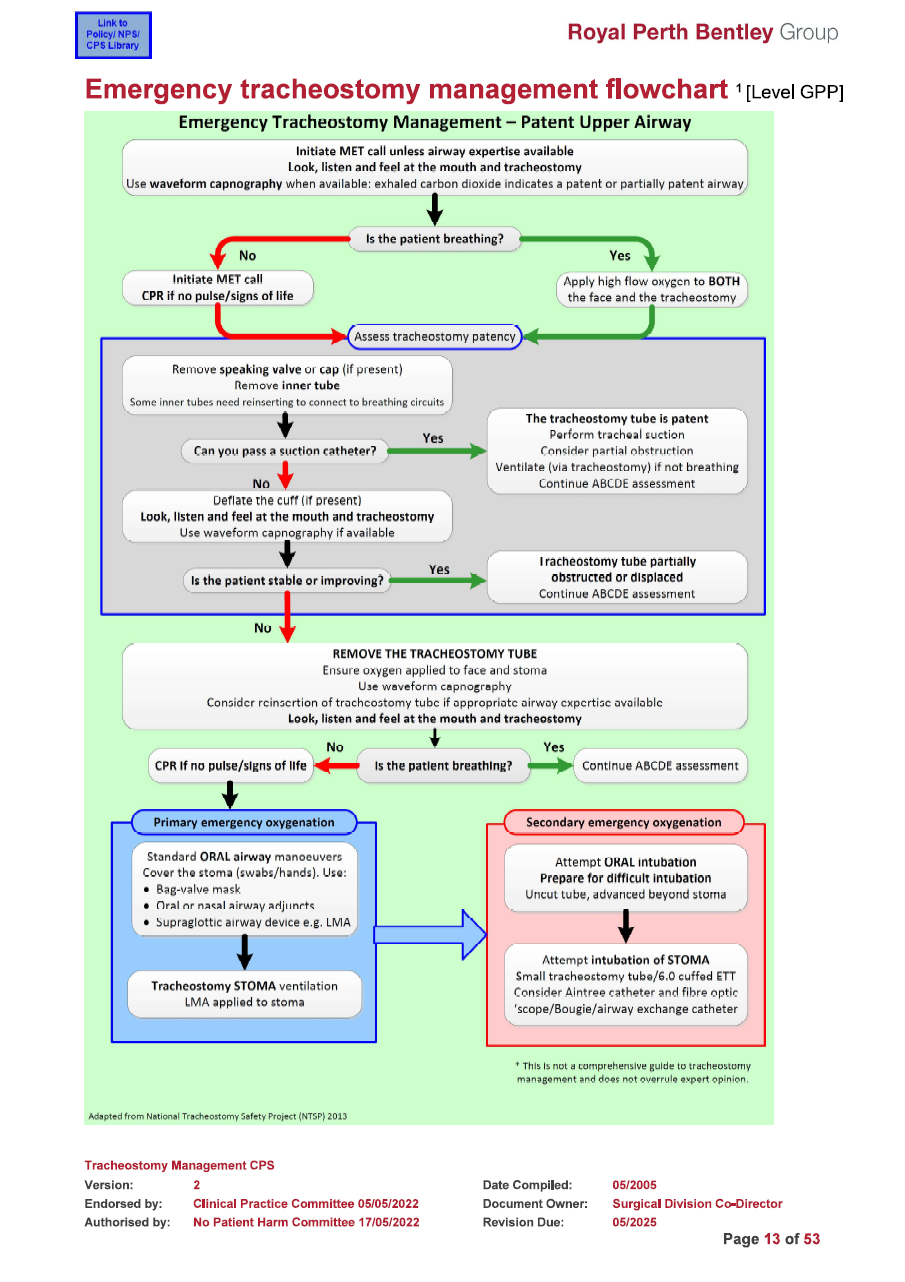
Unable to pass suction catheter
- The stoma or tube is likely to be totally blocked.
- If a tracheostomy tube is present, the tube may be displaced. If the tracheostomy tube has a cuff, deflating the cuff without removing the tube may partially correct the displacement and allow for spontaneous ventilation and oxygenation.
- Suction may be required following deflation as secretions collected above the cuff may be released into the lower airways.
No improvement / deterioration
- If unable to pass a suction catheter and cuff deflation has not led to improvement, the tracheostomy tube (if present) must be removed. Further attempts at troubleshooting are unlikely to be successful.
- Higher pressure may cause alveolar collapse, mucosal damage or catheter collapse, whilst inadequate suction pressure may not remove enough secretions resulting in increased number of catheter passes
- Appropriate PPE should be worn for suctioning
| Settings | |
|---|---|
| Extended Care: | |
| Colour assist: | |
Child and Adolescent Health Service (2020). Tracheostomy management. https://www.cahs.health.wa.gov.au/-/media/HSPs/CAHS/Documents/Community-Health/CHM/Tracheostomy-management.pdf
Royal Children’s Hospital. Tracheostomy Management. In: Clinical Nursing Guidelines, editor. Melbourne Australia: The Royal Children's Hospital Melbourne; 2018.
Perth Children's Hospital. Tracheostomy Management Guideline. In: Clinical Practice Manual, editor. Perth: Child and Adolescent Health Services; 2018.
Perth Children's Hospital. Tracheostomy Resuscitation Procedure. Clinical Practice Manual. Perth: Child and Adolescent Health Services; 2017.4.
Credland N. How to suction via a tracheostomy. Nurs Stand. 2016;30(28):36-8
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.