Cardiac Arrest is a time critical condition requiring immediate action and intervention.
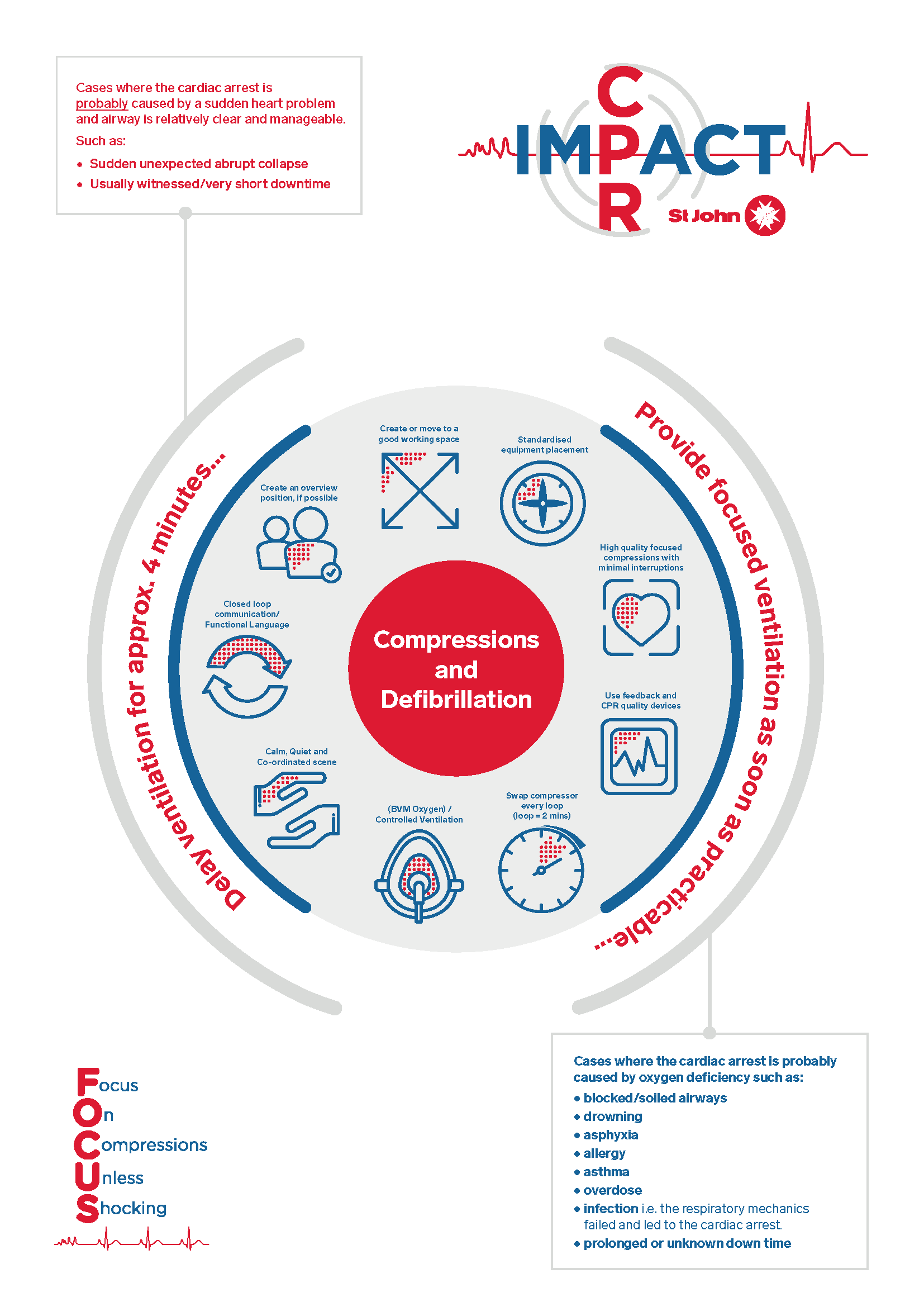
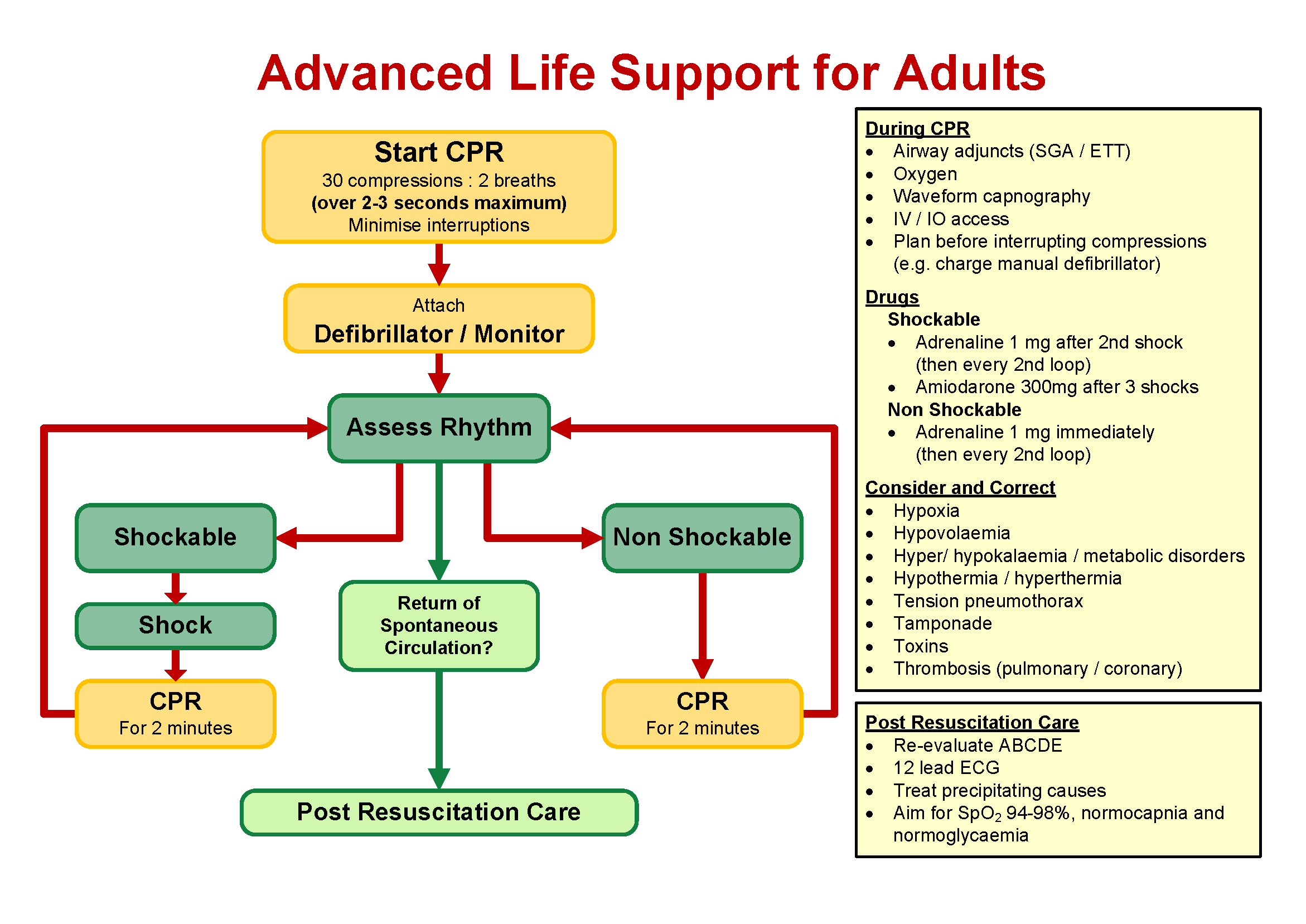
The ARC ALS algorithm provides a simple flow of needs for the cardiac arrest patient and provides the core components of an improved performance and CPR team resuscitation model - IMPACT (SJAWA version of high-performance CPR).
IMPACT is designed around a set of principles intended to make sure the quality of care is at its best and is being delivered by a high-functioning group of personnel who communicate well, interact well and prioritise actions as appropriate with task focus.
The main objectives of IMPACT are to ALWAYS:
- Provide consistent high-quality resuscitation with a focus on defibrillation, oxygenation and excellent compressions that are minimally interrupted
- Create conditions to optimise a shockable rhythm being successfully reverted.
- Have the mindset that achieving Return of Spontaneous Circulation (ROSC) as early as possible to influence survival with good neurological outcomes.
As soon as Cardiac Arrest is established, commence resuscitation unless the Determination of Death criteria are obvious. If in doubt, start resuscitative efforts until facts are established.
If circulation is restored, refer to Return of Spontaneous Circulation (ROSC) CPG.
- If trauma is the cause, follow the Traumatic Cardiac Arrest CPG
- “Sudden Cardiac Arrest” is defined as an unexpected and abrupt event in somebody who has been well up to the point of collapse or a very short time before that. Must be witnessed, heard or have a very short credible down-time.
- Take over compressions from bystanders on arrival.
- Early application of LUCAS (where available) is de-emphasised and should only be considered when a patient is being moved or transported.
- 30:2 is best regarded as 30 compressions to 2 seconds pause (to facilitate ventilation). Recommence CPR at 2-3 seconds regardless and do not wait for 2 breaths to be completed.
- Early preparation for transport is de-emphasised in most cases, except where there are compelling circumstances.
Commence High Quality, Task Focused, Minimally Interrupted Chest Compressions.
- CPR Feedback Devices are mandatory where available.
- Assess and defibrillate “Shockable” Rhythms every 2 minutes safely with a minimal peri-shock pause OR follow AED prompts.
- Oxygenate patients early:
- Passively via a high flow oxygen mask for 4 minutes in select patients OR
- Via controlled BVM ventilation as soon as practicable for all other patients (see circular diagram)
All passively oxygenated patients MUST be ventilated at approximately 4 minutes.
- As per Primary Care guidelines
- An i-gel® should be considered the first line adjunct in MOST cases.
- Do not attempt endotracheal intubation where a supraglottic device is adequate.
- Gain vascular access when possible to do so.
- Adrenaline as per CPG after 2nd shock (or ASAP after IV access has been established) and thereafter every 2nd loop.
- Amiodarone after a total of 3 shocks have been given (including AED shocks delivered prior to ambulance arrival).
- Fluid therapy as per CPG for hypovolemic cardiac arrest
- Work as a team, communicate well and establish a ‘hands-off’ overview position.
- As per Advanced Care guidelines
The treatment for Cardiac Arrest patients revolves around core requirements; excellent quality chest compressions that are never interrupted unnecessarily, timely defibrillation and oxygenation.
Traditionally, these care needs have been approached in a regimental manner, and often some skills are prioritised at the expense and quality of others. Prioritising the core elements is essential and apply each of the other principles around that as necessary – as soon as it is possible to do so.
There is no prescribed order for this; it is dynamic and circumstance dependant as reflected in the Circular Diagram below.
| Working space | Good resuscitation cannot generally be delivered in poor environments. A rapid and dynamic risk assessment should be done to either create space or move the patient. |
| Standardised equipment placement | The right equipment in the right place as often as possible. |
| High quality compressions | Focused compressions (attention to quality) that are minimally interrupted. The use of CPR Quality Feedback Devices (where available) is mandatory. |
| Swap compressor EVERY 2 MINUTES | A fatigued compressor delivers poor quality compressions. Prioritising paramedic skills over a swap of compressor in resource poor cases should not routinely occur unless it is critical to do so. |
| Create overview | Scene leadership should be established as soon as practicable. This person should NOT be delivering skills, and ideally be standing away. |
| Maintain a calm, coordinated scene | Encourage a calm and controlled scene with closed loop communication between the team, using functional language. |
| Ventilation | The use of a BVM should be viewed as an important task in providing controlled ventilation. Aim for correct rate without excessive volumes under pressure. |
Standard basic and advanced life support as detailed above is appropriate for the vast majority of adult patients. There are some situations where modified or additional management is required, as detailed below. Clinical judgement should always apply
when using these guidelines.
Paramedic Witnessed Cardiac Arrest:
- The Australian Resuscitation Council recommends early application and defibrillation shock where appropriate.
- In line with the Defibrillation skill staff trained and authorised may consider a 3-stacked shock approach in witnessed cardiac arrests where:
- The patient was well-oxygenated and perfused prior to the arrest
- The patient is in a shockable rhythm
- The first shock can be delivered within 20-seconds of the cardiac arrest occurring
- Manual mode is available and charging / rhythm recognition can be less than 10 seconds
- If the patient does not have a return of spontaneous circulation within 10 seconds of the third shock CPR should be immediately commenced
- For the purpose of timing medications and other interventions, stacked shocks are counted as a single shock.
Persistent shockable rhythms (refractory VF/pVT)
Where Ventricular Fibrillation or pulseless Ventricular Tachycardia persists despite three defibrillation shocks:
- Ensure defibrillator is charging to correct energy setting (200J for adults) and pad placement is appropriate as per Defibrillation skill
- Administer Amiodarone - 300mg IV/IO after third shock
- Consider alternative (anterior-posterior) pad placement as per Defibrillation skill
- Consider further Amiodarone - 150mg IV/IO after two further shocks post first Amiodarone (minimum five shocks)
- Consider ECMO suitability if available
- Consider double sequential defibrillation if two manual defibrillators available and specifically trained and authorised clinician present (clinical exception required)
- Consider Lignocaine - 1mg/kg IV/IO after two further shocks post second Amiodarone (minimum seven shocks) (clinical exception required)
Single Responder Resuscitation
Where a single responder clinician is the first at the scene of a cardiac arrest:
- Attach cardiac monitor/defibrillator or AED immediately. It is acceptable to use a manual defibrillator in automatic mode until additional clinicians arrive
- Perform CPR with a focus on high quality chest compressions, utilising mechanical CPR if available or bystanders to help
- Interventions such as vascular access, medications or airway management are not a priority and should only occur prior to the arrival of further clinicians if they do not interrupt high quality CPR.
Mechanical CPR
Mechanical CPR does not usually have a role in immediate management of cardiac arrest as there is no evidence it routinely improves outcomes or is of better quality than high performance manual CPR. However it should be considered when:
- There is insufficient space or clinicians to perform manual resuscitation safely or effectively
- Clinicians are fatigued and prolonged resuscitation attempts are expected
- Extricating and transporting a patient with ongoing resuscitation attempts
Mechanical CPR should be applied in a manner that minimises pauses to chest compressions.
A trained and authorised clinician must be present to supervise the mechanical CPR device whenever in use.
Termination of Resuscitation
Cardiac arrest in special circumstances
CPR Induced Consciousness (CPRIC)
A patient may move or show other signs of life while in cardiac arrest if cerebral perfusion is maintained with high quality CPR. This situation may lead clinicians to believe the patient is not in cardiac arrest and lead to delayed defibrillation and/or inappropriate pauses in CPR.
If is patient movement or other signs of life in cardiac arrest:
- It is appropriate to briefly pause CPR to confirm whether the patient is still in cardiac arrest or whether ROSC has been achieved.
- If the patient remains in cardiac arrest, resuscitation attempts should be continued.
- If the patient's movement is significant enough to interfere with resuscitation, consider ASMA consult for discussion of sedation options.
Cardiac arrest in pregnancy:
- Manual Uterine Displacement to relieve aortocaval compression
- If this is not possible, place padding, such as a towel, under the right hip to tilt the patient’s hips approximately 15-30°
- Consider rapid extrication and transport for resuscitative hystorotomy
- Consider transport to ECMO capable facility
| Settings | |
|---|---|
| Extended Care: | |
| Colour assist: | |
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.