
If there is any doubt about the following criteria or it is not obvious – commence resuscitation;
- Decomposition, larval infestation or putrefaction
OR
- Signs of Rigor Mortis OR Gravitational Dependent Post-Mortem Hypostatis in association with Determination of Death criteria
OR
- Major traumatic injuries incompatible with life; for example:
- Decapitation, Significant Cranial destruction, Significant Truncal destruction
- Hemicorporectomy / trans-lumbar amputation
- Obvious Injuries with Exsanguination or Profound blood loss inconsistent with life
- Document ALL relevant findings carefully
OR
- Major Incidents / Multi Casualty situations where clinical resources are overwhelmed, and applied Triage Pack guidelines indicate death/futility of a victim with no signs of life
When recognising life extinct, a Determination of Death must be made with the following criteria:
- No Central Pulses at all and
- Asystole for >30 seconds[1] and
- Fixed and Dilated pupils with NO corneal reflexes at all and
- No signs of Breathing at all and
- No Auscultated Heart Sounds (if in scope of practice)
Some pacemaker spiking activity may be observed for some time after death. If an AED is used, it must have ‘No Shock Advised’, especially if there is no screen on the device. Have a low threshold for seeking advice
from Clinical Support Desk where necessary.
Refer to Supplementary Notes for Deceased Persons if necessary
There may be circumstances where the commencement of resuscitation may be unwanted or very unlikely to reverse the situation favourably, unless there are compelling reasons or special circumstances. Determination of Death should be followed thereafter.
If there is any doubt about the following criteria or it is not obvious– commence resuscitation;
- Prolonged Cardiac Arrest (i.e. estimated downtime greater than 15 minutes) and
- Generally unwitnessed and
- First assessed rhythm is Asystole and
- Not received a defibrillation shock and
- No compelling reasons or special circumstances to continue
Expected Deaths / Advanced Directives;
- There is credible evidence that death was expected as a result of terminal illness
- The individual has taken the Voluntary Assisted Dying substance
- It is the patient’s wishes not to be resuscitated and have previously been clearly communicated and this seems reasonable to attending St John staff. It is not necessary to sight an advanced directive[2]
Residential Care Facility[3] patients who;
- Are aged 80 years or over and
- Obviously frail (Frailty Score 7, 8 or 9).
Patients in the Community with ALL the following
- Aged 80 or over with
- Asystole as the presenting rhythm, and
- Clearly frail (Frailty Score 7,8 or 9) - most will have life-limiting co-morbidities e.g. Chronic Renal Failure, Advanced Dementia or Cerebrovascular disease, Hemiplegia, Advanced COPD, Chronic Cardiovascular disease.
If the criteria for ROLE or Withholding resuscitation are subsequently met, then efforts for those patients may be terminated and Determination of Death can be made.
When Special Circumstances or Compelling Reasons to continue are identified, efforts should be extended (e.g. younger age, refractory VF/ recurrent arrest or timely access to ECMO.). Any decision to terminate should be made very cautiously and discussed with Clinical Support Desk and / or ASMA.
In other cases, maximally directed resuscitation must be continued. However, it is recognised there will be occasions when resuscitation efforts may be considered futile.
Sound clinical judgement and reasoning should always apply and take into consideration many factors and prognostic indicators.
Termination of Resuscitation may apply if;
- The presenting rhythm is Asystole, not SJA witnessed, and remains in Asystole after 20 min of maximally directed resuscitation
OR
- The presenting rhythm is shockable, not SJA witnessed, and progresses quickly and remains in, Asystole OR wide, slow PEA (<40/min) after 20 – 30 mins with NO other favourable signs of response to efforts (e.g. high EtCO2)
OR
- The destination ED is > 15 minutes away from the arrest location, 20 minutes or more of maximal BLS/ALS has been applied, ROSC has not been achieved at any stage and there are no special circumstances or other compelling reasons to continue.
OR
- A specifically authorised SJA clinician makes a reasonable decision based upon prognostic futility either on scene or via the Clinical Support Desk or ASMA.
OR
- Prolonged CPR in Blunt Traumatic Cardiac Arrest after reversible causes have been addressed is almost never associated with a good outcome. If delivery to an ED cannot be achieved within 25 minutes from arrival on scene, it is reasonable to terminate resuscitation if NO ROSC is achieved after 10 minutes, and Determination of Death criteria are met.
If in doubt, contact the Clinical Support Desk. Volunteer Crews should have a low threshold to do so.
PEA associated with a rhythm that is compatible with cardiac output may indicate a “low-flow” or "pseudo-PEA" state where cardiac output is present but insufficient to produce a palpable central pulse. In this setting, have a very low threshold for consulting with the Clinical Support desk and/or ASMA for further management advice.
Any Termination of Resuscitation in patients with a PEA presenting with a narrow complex and/or a rate of 40 beats per minute or higher must have a consultation with a Clinical Support Paramedic and/or ASMA prior to termination of efforts.
Refer to Supplementary Notes for Deceased Persons if necessary
The decision to terminate resuscitation efforts requires sound judgement. Determining the likely cause of the cardiac arrest and good background history is important. There is no specific or absolute time for a decision to be made as each case will be different.
| C | Cause / Special circumstances / compelling reasons– e,g, Sudden collapse of presumed cardiac origin, overdose, asphyxia, drowning, pregnancy etc. – would all favour prolonged resuscitation / transport to ED |
|---|---|
| R | Resuscitative Effectiveness – e.g. Good CPR quality measured via feedback device, CPR induced femoral pulses, EtCO2 fluctuations, Refractory or Recurrent VF – would all favour prolonged resuscitation |
| A | Ask and include the team |
| F | Futile features – e.g. Time in arrest, unresponsive to resuscitation, poor EtCO2, slow PEA or agonal activity, co-morbidities, neurological functional status, frailty / physiological reserve to recover and ICU admission likelihood – would favour termination |
| T | Transport, Time and Handling risks – e.g. Is it feasible and safe to move and transport the patient? Consider bariatric features, location and time to ED, public place, etc. |
| E | Explain and engage with family or other necessary parties – Families should not necessarily be asked whether efforts should cease as they are often unprepared. Be empathetic, tactful and honest. Provide support to them in their time of loss |
| D | Document rationale for decisions clearly and fully |
Prognostic Indicators
| Less Favourable | More Favourable |
|---|---|
| Prolonged down time | Shorter down time |
| Unwitnessed | Witnessed |
| Non-Shockable presentation | Shockable presentation |
| No bystander CPR | Bystander CPR |
| No AED Shock | AED Shock |
| EtCO2 values falling | Normal / High EtCO2 |
| Wide Complex PEA | Narrow Complex PEA |
| Advanced Frailty | Low Frailty |
| Older (> 80 y/o) less likely to admit ICU | Younger more likely to admit ICU |
| Significant Co-Morbidities | Less significant Co-Morbidities |
A Medical Practitioner may certify Life Extinct. They may also issue a Cause of Death Certificate where they believe the death had a known cause and the deceased is known to them.
Ambulance Officers may certify Life Extinct under the provisions of the Coroner. A Life Extinct Form, electronic or paper, is required for any deceased patient that SJA attends.
In Voluntary Assisted Dying cases:
- Any handwritten / hard copy life extinct form must not be notated to reflect VAD; this is a legal requirement. Reference to expected death or advanced directive will be sufficient if at all.
- ePCR life extinct forms should ordinarily have the option relating to advanced directive selected.
Reportable Deaths: Deaths in these categories require notification to the coroner.
- Appears to have been unexpected, unnatural or violent or to have resulted, directly or indirectly, from injury.
- Person who immediately before death was a person held in care. (*)
- Appears to have been caused or contributed to by any action of a member of the Police Force.
- A person whose identity is unknown.
(*) The term “person held in care” means a person held:
- Under the Child Welfare Act.
- In custody under the Prisons Act.
- In any centre under the Alcohol and Drug Authority Act 1974.
- As an involuntary patient or apprehended or detained within the meaning of the Mental Health Act 2014.
- As a detainee under the Young Offenders Act 1994.
An important point to understand is that once the decision has been made to report the death to the Coroner, all evidence of medical intervention in the deceased must remained untouched. This means that all tubes, intravenous lines and other aspects of medical intervention must be left in situ as these could be examined in detail. In the case of children, the endotracheal tube may be cut off at the lips if there is to be a viewing of the body.
Obvious Deaths:
This is the only category in which Police Officers may/will issue a Life Extinct form.
Suspicious Deaths:
Suspicious deaths may include criminal acts, suicides, stabbings, shootings, overdoses or where the information gathered does not make sense. Where Officers suspect a suspicious death Police need to be called immediately and the scene secured. Documentation is important and any details you gather should be included. This is evidence and may be required by a court. Patient care to others should not be delayed. If CPR is stopped please leave the scene as is. Should this happen Officers need to be aware that they will contribute to evidence at the scene and may inadvertently contaminate the scene. In cases of a hanging; the knot used to form a noose should be left tied and the rope cut away from the knot where possible. Do not cut down the deceased if there is an obvious death and CPR is not considered.
Non Suspicious Deaths:
Non suspicious circumstances may include deaths at home of natural causes. If there are no suspicious circumstances, the Medical Practitioner may be phoned and once given the circumstances surrounding the death asked if a Cause of Death Certificate will be forthcoming. If so there is no need to contact Police. The relatives may then be advised to contact a funeral service of their choice and make all further arrangements. The name of the Medical Practitioner and time contacted must be documented. Should the deceased’s Medical Practitioner be unavailable or a Death Certificate is not forthcoming, then the Police must be called and advised of the situation. Officers may be required to take the deceased to the mortuary on request of police.
Wellbeing and Support Services:
Officers who attend these deaths might find themselves reacting to these potentially traumatic events and may need to contact Wellbeing and Support. This service is available to all frontline staff, 24 hours per day.
Many people, especially relatives, may also require some support. They should be signposted, based on the situation, to the St John WA bystander card (available at depots) and/or to their GP for additional support.
Complete list of Support & Resources available here.
- Community Services are available on the bystander card
- If it’s an MVA; Road Trauma Support WA is available
- if it’s a suicide; Lifeline, Suicide Call-back Line and Beyondblue (depression) are good resources
- Mental Health Emergency Response Line (1300 555 788) is useful in several situations
Wellbeing and Support:
All hours contact: 08 9373 3827
wellbeingandsupport@stjohnwa.com.au
Key Terms & Links
Dalhousie Clinical Frailty Scale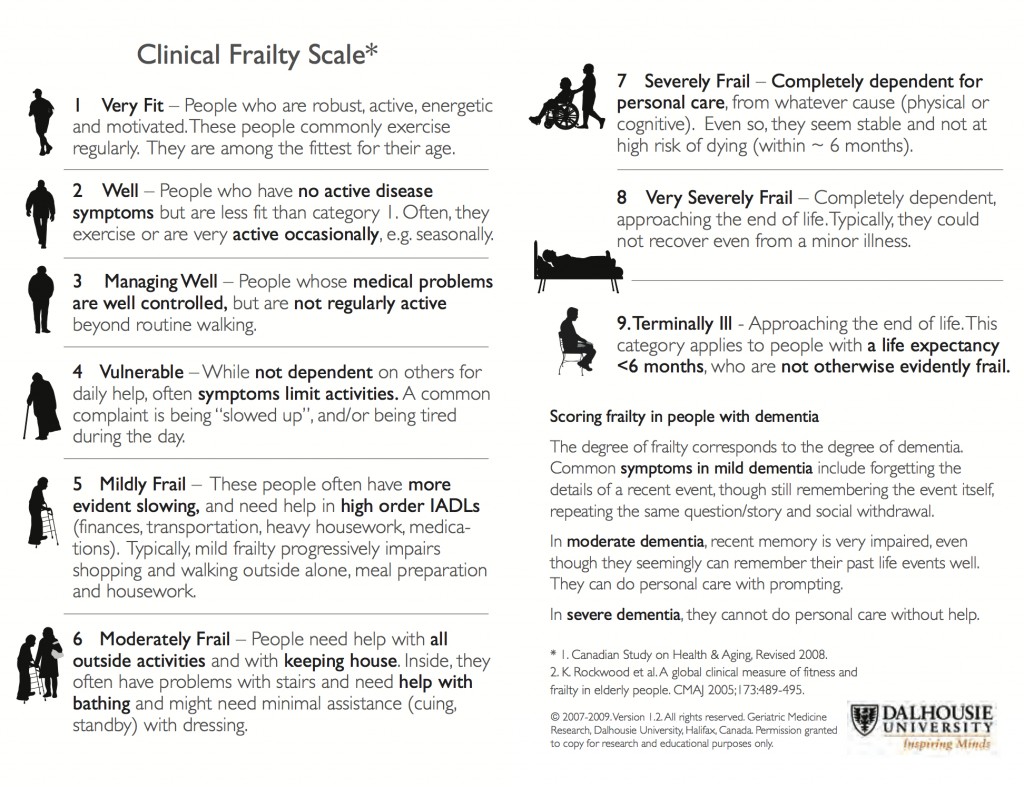
[1] There will be occasions where some activity of a dying heart can be observed. These are most commonly defined as very wide, disorganised and extremely slow complexes. Wait for this to deteriorate to Asystole. This may take several minutes and Determination of Death can be made thereafter.
[2] These do not have to be in writing, and can be communicated to St John staff verbally as long as it is from a trusted / credible source. Refer to the Guardianship and Administration Act 1990.
[3] This is an end of life event. These patients may be in a shockable rhythm but all have extremely poor outcomes regardless of presenting rhythm.
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.