- Stroke occurs when arterial blood supply to the brain is suddenly disrupted due to obstruction by a thrombus or plaque (Ischaemic stroke 85%), or because an artery ruptures (Haemorrhagic stroke 15%).
- Transient ischaemic attack (T.I.A.) is also significant as it may precede a stroke.
- Maintain a high index of suspicion of cerebrovascular accident in persons presenting with neurological symptoms over the past 24 hours, excluding obvious causes for these neurological symptoms such as hypoglycaemia.
Read the complete article; Stroke in the Medical Library > Pathophysiology.
Patients who present with any of the following should be assessed for a cerebrovascular accident:
- Weakness, numbness or paralysis of the face, arm or leg (unilateral or bilateral)
- Dysphasia, language difficulties
- Dizziness, ataxia, loss of balance or an unexplained fall
- Loss of vision, visual field disturbances, double vision, or sudden blurred or decreased vision in one or both eyes
- Headache, usually severe and of abrupt onset
- Dysphagia, difficulty in swallowing.
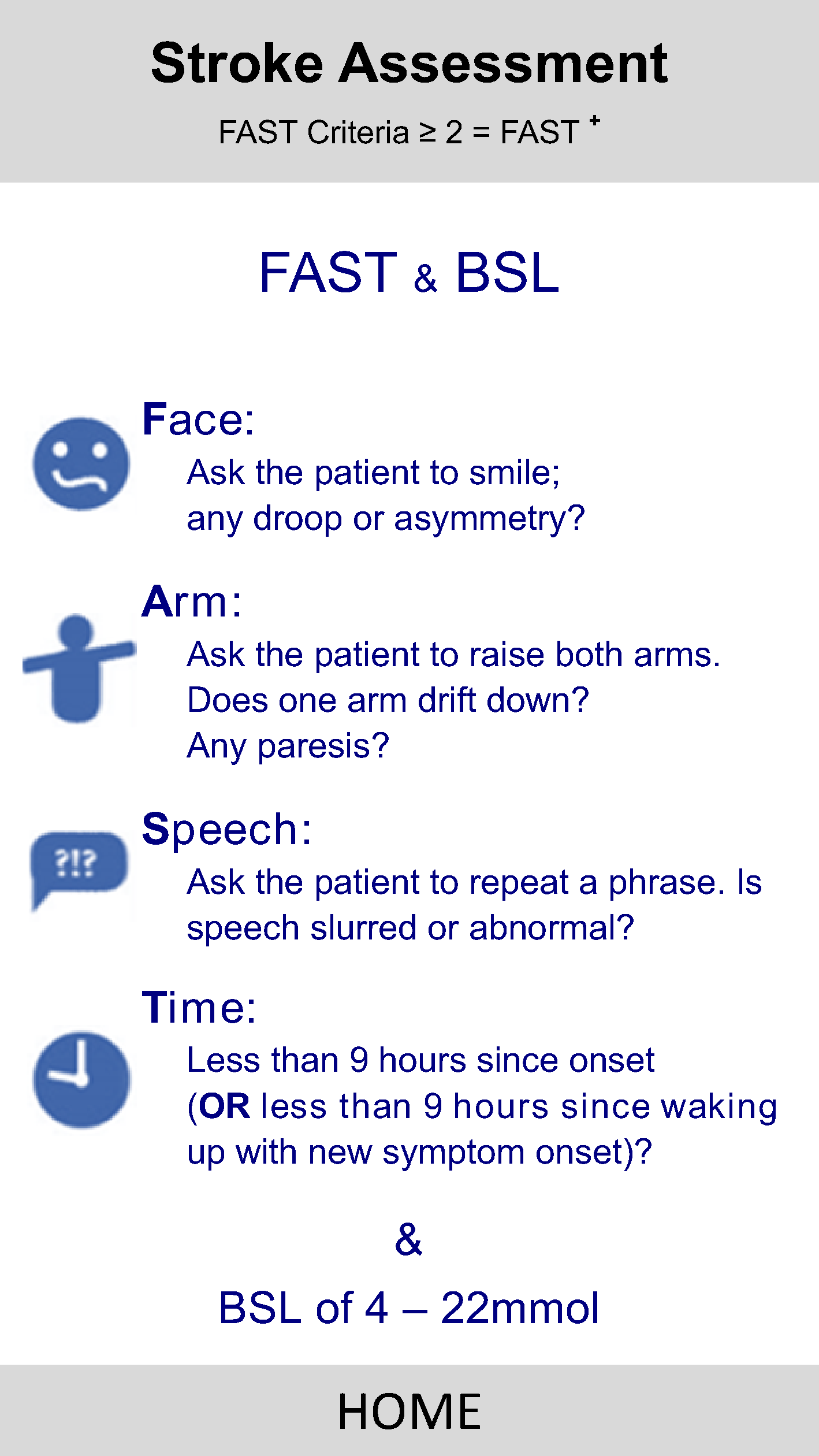
- FAST (Face, Arm, Speech and Time) is a rapid diagnostic tool for the evaluation of stroke like symptoms.
- If 1 or more abnormality exists (to Face, Arms or Speech), and symptom onset is ≤ 9 hours (Time), then the patient is considered FAST+.
- Time is measured from symptom onset & must be ≤ 9 hours for patient to meet the FAST+ criteria.
- If the patient has woken with stroke symptoms (but was asymptomatic prior to sleeping), time starts from waking up.
Patients who are FAST negative may still be having an acute CVA, and a thorough neurological assessment should be performed
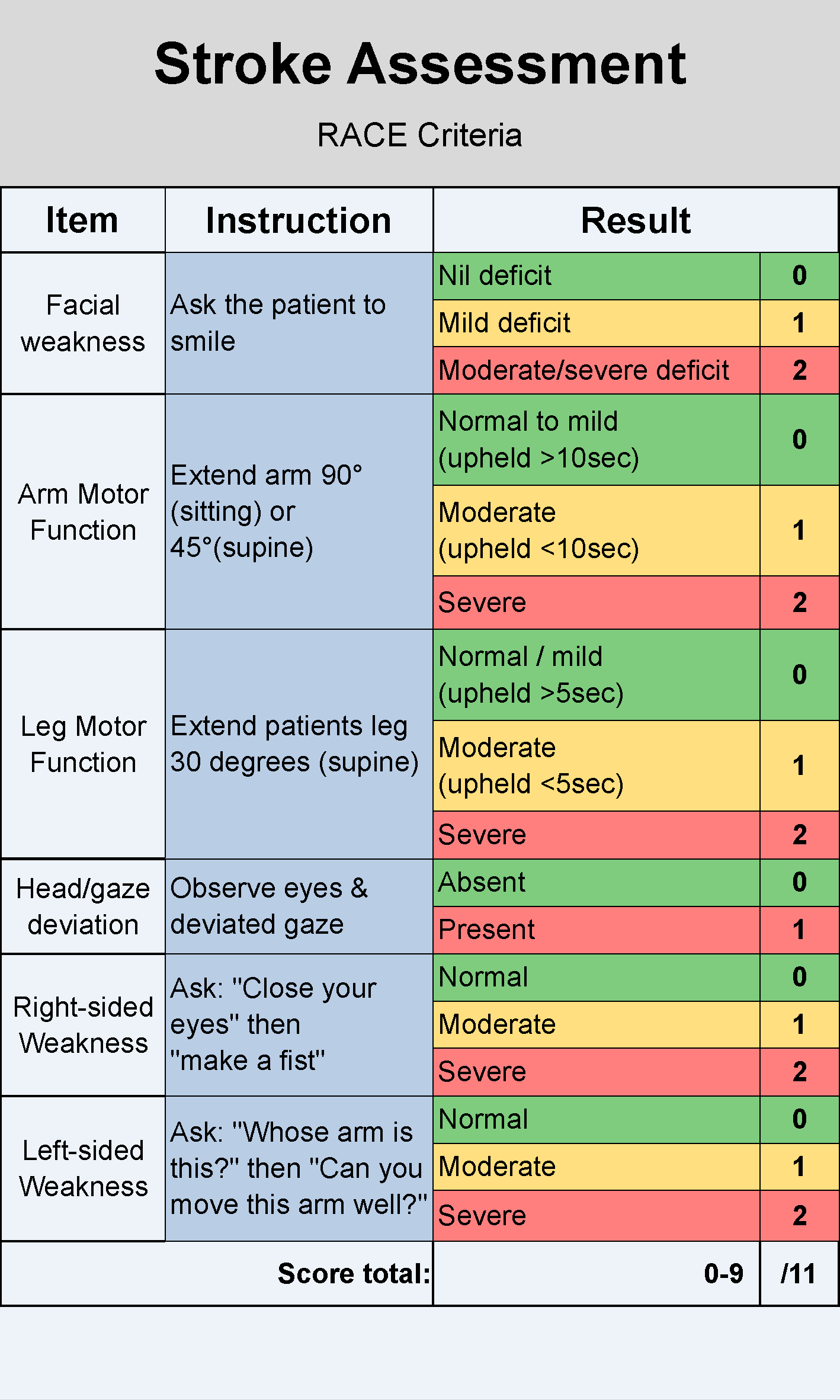
- RACE (Rapid Arterial oCclusion Evaluation) is a quantifying tool used to assess the likelihood of a large vessel occlusion and identifies the patients’ that may require urgent neuroendovascular clot retrieval.
- TIA (Transient Ischaemic Attack) symptoms may resolve completely within minutes to hours of onset, but are still indicative of an at-risk patient. These patients require assessment at a stroke centre.
- Improved stroke patient outcomes rely on:
- Rapid on-scene assessments
- Early ED, ASC or ANU notification
- Urgent transportation
- Information gathering, inclusive of time of onset/last seen well and next of kin details
- Rapid on-scene assessments
RACE Calculator
An online RACE Assessment calculator to establish a RACE score.
- Complete Primary Survey
- Open, clear and maintain the airway
- Oxygen if indicated
- Complete Vital Sign Survey, including BGL
- Consider applying cardiac monitor if trained and authorised
- Conduct FAST assessment; if FAST+, stroke is the likely diagnosis.
- Conduct RACE assessment to identify Large Vessel Occlusion (LVO).
- If stroke bypass criteria is met, transport to appropriate destination as indicated
- If stroke bypass criteria is not met, transport to nearest ED
- Cardiac monitoring
- Conduct FAST assessment;
- If FAST- but history is suggestive of TIA, the patient is at risk and still meets stroke bypass criteria
- If FAST+, stroke is the likely diagnosis; conduct a RACE assessment to identify Large Vessel Occlusion (LVO).
- Obtain IV Access (ACF preferable)
- Collect pre-hospital blood sample
- Aim for on scene time < 15 minutes
- If stroke bypass criteria is met, transport to appropriate destination as indicated
- If stroke bypass criteria is not met, transport to ED as directed by ANC, or nearest ED if urgent intervention is required
- As per Advanced Care guidelines
| Inclusion Criteria | ||
|---|---|---|
| ||
| Acute Stroke Centre | Acute Stroke Centre | Acute Neuroendovascular Unit |
Transient Ichaemic Attack | For patients FAST+ | For patients FAST+ and with RACE ≥ 5 |
| Transport via normal road conditions | Transport Priority 1; pre-notify hospital via ED patch line | |
Monday - Sunday, 24 hours a day |
| |
Regional Centres
| ||
- Specified inclusion criteria are not met.
- An urgent intervention is required at closest ED.
Possible complications / outcomes of stroke:
- Permanent Disability
- Brain damage
- Death
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.