- A burn is an injury caused by thermal (e.g. heat) and non-thermal (e.g. electrical) causes. This guideline encompasses burn injuries caused by electricity, heat, chemicals, light, radiation or friction.
Tertiary Burns Centre:
- Adults: 16 years and over - Fiona Stanley Hospital (FSH)
- Paediatrics: 15 years and under - Perth Children's Hospital (PCH)
- Assess airway burns for:
- Soot in nasal and mouth cavities
- Cough and hoarseness
- Black sputum
- Difficulty in breathing and swallowing
- Blistering around mouth and tongue
- Scorched hair, eyebrows or facial hair
- Document the time of burn injury;
- Assessment of the patient includes inhalation injury; % TBSA affected; site and depth of wounds; the patient’s age; the presence of other injuries, the mechanism of injury; any areas of circumferential burns, co-morbidities and psychosocial issues;
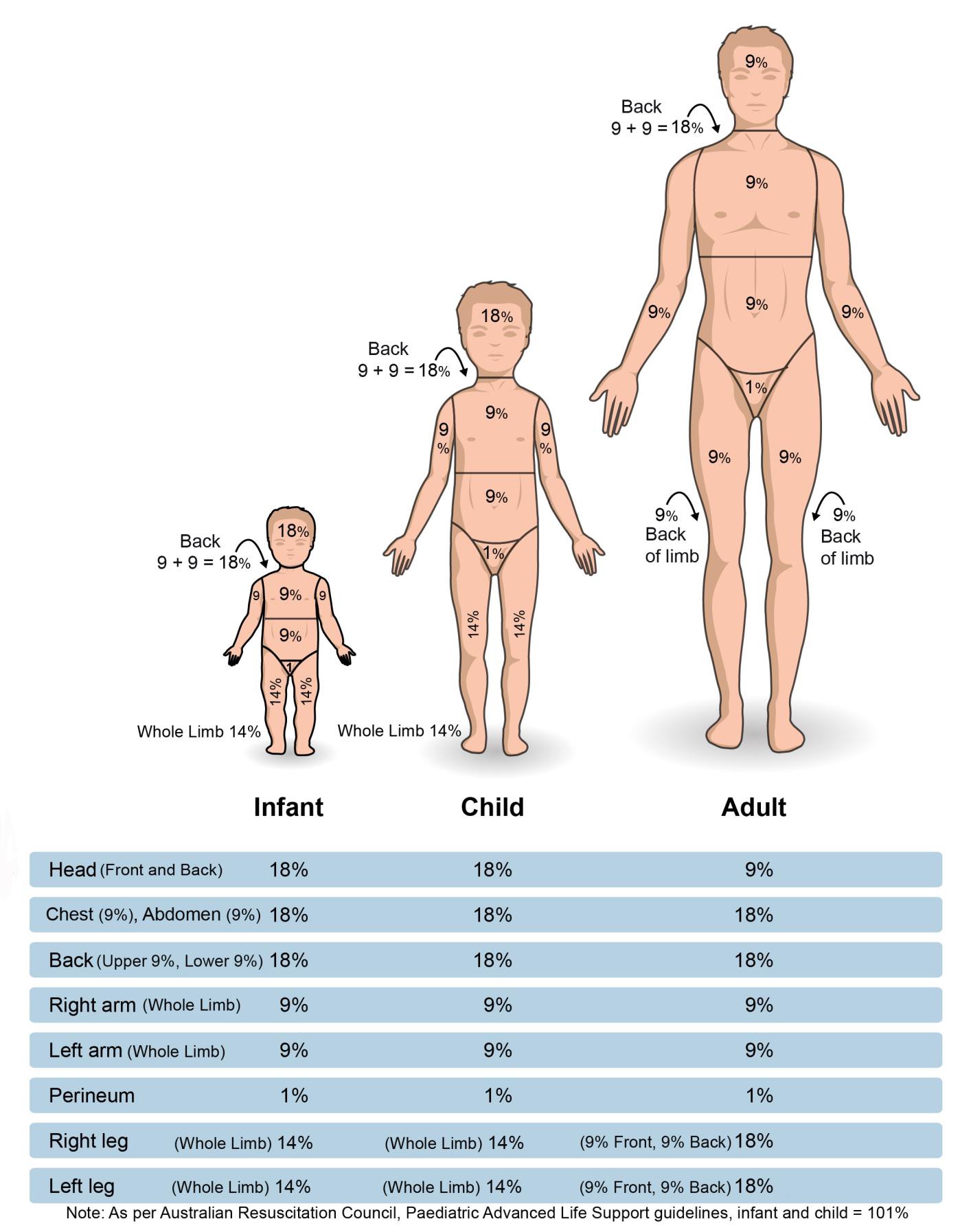
- Reddened and intact skin areas should not be included when calculating % TBSA burnt;
- There may be entry and exit point for electrical burn injuries;
- Patient suffering electrocution injuries should be monitored for dysrhythmias and 12-lead ECG performed;
- Hydrogel dressings can be applied in the absence of water to cool, but this is not preferred.
- When cooling the patient, be careful to avoid hypothermia - optimal water temperature is 15°
- Primary Survey with c-spine consideration
- Be aware of Trauma Management Principles
- Airway management/ventilatory support (as required)
- Oxygen therapy (note: carbon monoxide inhalation may provide false SpO2 readings)
- Burn injury assessment (Rule of 9’s)
- Cool burn area for a minimum of 20 minutes
- Remove jewellery and clothing unless adhered to wound
- Apply damp sterile dressings after cooling and/or hydrogels
- Perform Vital Sign Survey
- Secondary / CNS Survey
- Salbutamol as required as per CPG
- Administer pain relief
- Consider applying cardiac monitor if trained and authorised
- Consider direct transfer to Tertiary Burns Centre:
- ≥ 10% TBSA burnt or >5% TBSA burnt paediatrics
- Airway burns
- Burns to face, hands, feet, perineum, genitalia
- Monitor patient closely, recording full observations every 10 minutes (or 5 minutes if time critical)
- Transport Priority 1 if patient time critical, pre-notifying receiving facility
- Salbutamol as required as per CPG
- Establish vascular access, administer fluid replacement as per below chart:
- Administer pain relief
- Consider cardiac monitoring
- Consider debridement:
- Perform Hand Hygiene, don clean gloves
- Wipe away dead skin/non-viable tissue and blisters with non vigorous rubbing if patient condition allows and appropriate analgesia has been administered.
- Consider direct transfer to Tertiary Burns Centre:
- ≥ 10% TBSA burnt, or >5% for paediatrics
- Airway burns
- Burns to face, hands, feet, perineum, genitalia, joints or neck
Fluid replacement indication criteria:
| Adults | >15% TBSA |
|---|---|
| Children 18 months and older | >10% TBSA |
| Children less than 18 months | >8% TBSA |
Formula:
| 2ml x %TBSA burn x weight of patient | 50% of total amount over the first 8 hours |
|---|---|
| 50% of total amount over next 16 hours |
- Fluid is calculated from time of burn injury, not from arrival on scene
- Monitor patient closely, recording full observations every 10 minutes (or 5 minutes if time critical)
- Transport Priority 1 if patient time critical, pre-notifying receiving facility
Parkland Calculator
An online calculator to assist in determining fluid administration for burns.
- Consider MEQU Fluid & Blood Warmer for intravenous fluid replacement.
- Elevate all affected areas when possible to reduce oedema and infection risk
- Inhalation of superheated smoke, steam or gases can induce airway oedema and rapid deterioration of airway patency.
- The risk of inhalation injury increases if the patient was exposed to burn source within an enclosed space
- Debridement may improve accuracy of TBSA calculation, and reduce risk of oedema and infection
- Compartment syndrome; signs of ischaemia include:
- Pain
- Pallor
- Paresthesia
- Pulselessness or >2 seconds CRT
- Cool or cold limb
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.