
Umbilical cord prolapse is an obstetric emergency occurring in 0.2-0.4 of births.
- Funic presentation (umbilical cord presentation; Figure A)
- The umbilical cord lies in front of the presenting part, the membranes are intact
- Overt umbilical cord prolapse (Figure B)
- The cord lies in front of the presenting part and the membranes are ruptured
- Occult umbilical cord presentation/prolapse (Figure C)
- the cord lies trapped beside the presenting part, rather than below it
If the cord is visible at the vaginal opening after the membranes have ruptured. This should be considered in all women at high risk for cord prolapse;
- Malpresentation
- Low birth weight
- Multiple gestation
- Multiparity
- Preterm Labour
- Abnormally long umbilical cord
- Delays in recognition and management are associated with significant perinatal morbidity and mortality due mainly to complications associated with preterm birth and birth asphyxia. Therefore, cord prolapse requires urgent intervention and assistance.
- During emergency ambulance transfer, the knee–chest position is potentially unsafe, the exaggerated Sims position should be assumed (left lateral with pillow under hip).
- Handling the cord risks continued cord compression and vasospasm.
- Note the time of cord presentation, as the hospital will need this information.
- Primary Survey
- Offer continuous support and reassurance
- Do NOT touch the cord or push the cord back in
- Position patient appropriately: Place the mother in a knee to chest position (Figure D) and transport in the exaggerated sims position ( Figure E) to keep fetal presenting part off the cord
- Cover the mother with a sheet/blanket to maintain dignity and body heat.
- Perform vital sign survey
- Consider oxygen if indicated as per CPG
- Apply cardiac monitor if trained and authorised
- Consider pain relief
- Consider anti-emetic
- If birth is imminent and the mother is actively pushing, deliver the baby as soon as possible as per Childbirth clinical skill:
- Prepare for newborn resuscitation
- Monitor patient persistently, recording full observations every 10 minutes (or 5 minutes if time critical)
- Transport Priority 1 immediately as this requires immediate C-section. Provide early notification to the receiving unit to enable preparation.
- Apply cardiac monitor if trained and authorised
- Establish vascular access
- Consider pain relief
- Consider anti-emetic
- If birth is imminent and the mother is actively pushing, deliver the baby as soon as possible as per Childbirth clinical skill:
- Prepare for newborn resuscitation
- Monitor patient persistently, recording full observations every 10 minutes (or 5 minutes if time critical)
- Transport Priority 1 to emergency obstetric unit immediately as this requires immediate C-section. Provide early notification to the receiving unit to enable preparation.
- As per Advanced Care (AP) guidelines
- Liaise with obstetrics unit in the metropolitan area, recording all advice on ePCR
- Liaise with local hospitals in country areas, recording all advice given on ePCR
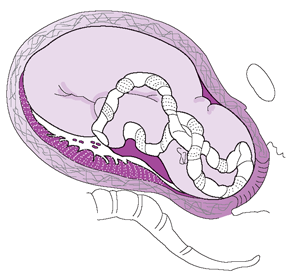 Figure A: Funic Presentation
Figure A: Funic Presentation
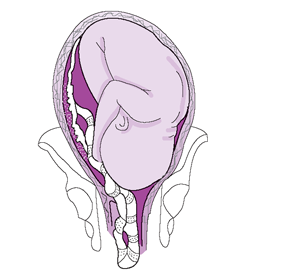 Figure B: Overt Prolapse
Figure B: Overt Prolapse
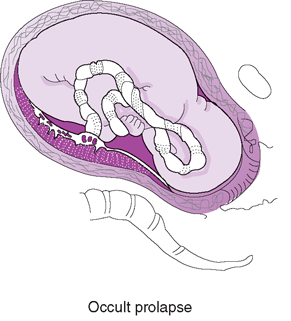 Figure C: Occult Prolapse
Figure C: Occult Prolapse
 Figure D: Knees to Chest
Figure D: Knees to Chest
 Figure E: Exaggerated Sims Position
Figure E: Exaggerated Sims Position
| Settings | |
|---|---|
| Extended Care: | |
| Colour assist: | |
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.