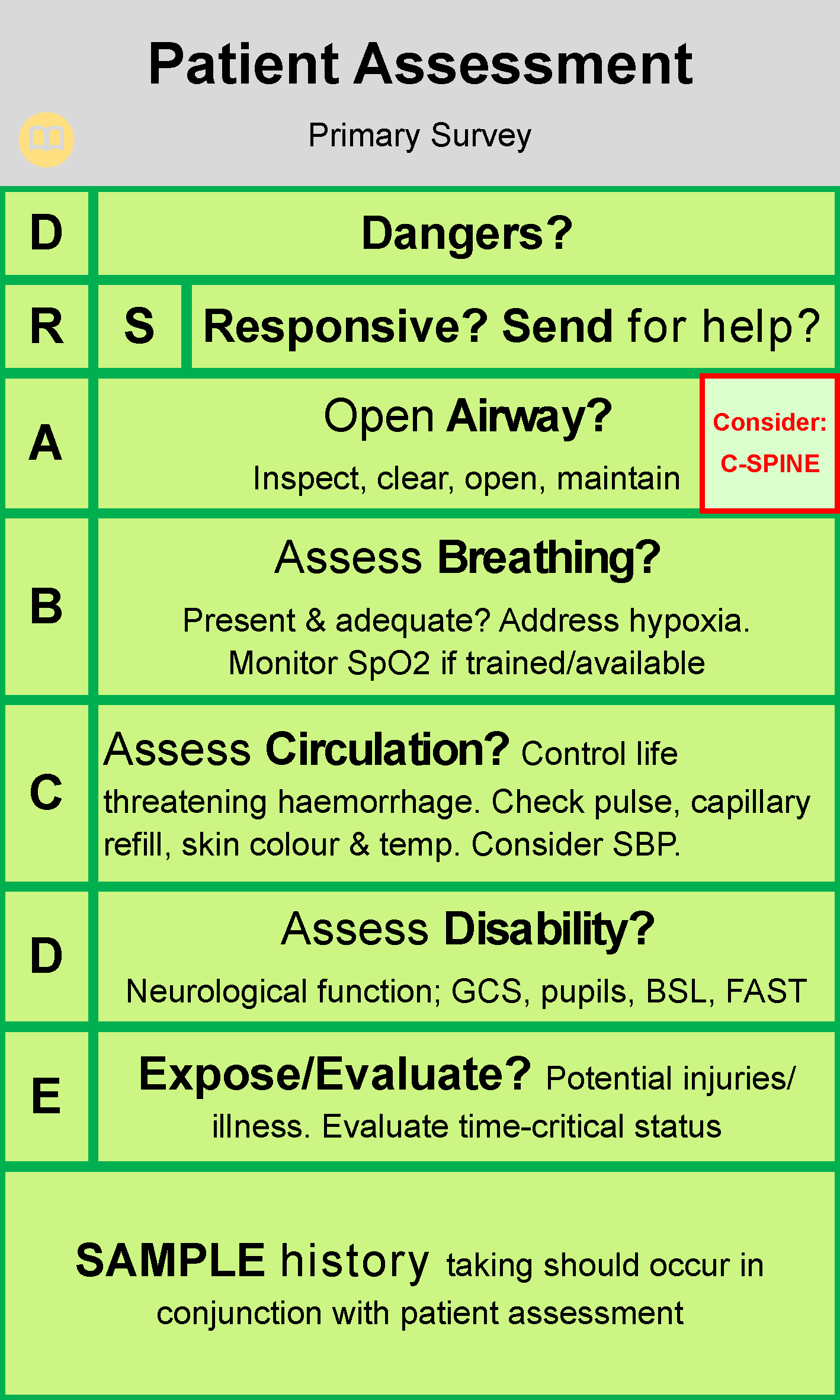
- The Primary Survey, or initial assessment, is designed to help the emergency responder detect immediate threats to life. Immediate life threats typically involve the patient's airway, breathing or circulation, and each threat is corrected as it is found. Life threatening problems (e.g. catastrophic haemorrhage) MUST be identified first.
- Always ensure scene safety prior to approaching patient to being primary survey
AIM: To detect and correct life threatening illness or injury.
Danger
Position the ambulance appropriately, taking into consideration patient access and egress.
- Don appropriate PPE.
- Approach scene cautiously.
- Assess for dangers to self, partner, bystanders and patient. Look, listen and smell to identify potential or existing hazards present. Evaluate risks and negate danger if safe to do so.
- Consider need for other emergency services required to ensure scene safety (WA Police, DFES, SES).
- If the patient is in immediate danger and they can be moved safely, do so at this stage, regardless of injury.
- Do not enter scene until deemed safe.
- If multi-casualty incident is evident, refer to the Emergency Management Guidelines
Response
- Perform a brief neurological assessment to establish patient’s conscious state (AVPU).
- Alert = Describes a patient who is spontaneously awake and aware of their surroundings.
- Verbal = Describes a patient who responds to verbal stimuli i.e. when spoken to in a loud voice.
- Pain = Describes a patient who responds to touch or a painful stimuli (trapezius squeeze only)
- Unresponsive = Describes a patient who does not respond to verbal or painful stimuli.
Send for Help
- Establish need for emergency services back-up:
- Consider how many patients there are at the scene, and their condition
- Are additional ambulances required?
- Are the Police and/or Fire/Rescue services required to help manage scene safety?
- Establish need for Clinical Support to assist with patient management:
- Clinical Paramedic: Contactable 24/7 in State Ambulance Operations Centre – referred to as CSPSOC.
Airway
- Open mouth using cross-finger technique.
- Inspect oral cavity for any obstruction and/or fluid.
- Clear airway with lateral position to assist drainage, finger sweeps, and/or suction.
- Open the airway by performing an appropriate airway manoeuvre:
- Triple – non injured adult patient
- Double – spinal injured adult patient
- Neutral alignment – Paediatric patient
- Maintain: Consider Oropharyngeal Airway (OPA) or Nasopharyngeal Airway (NPA) if unresponsive/appropriate.
- Place in lateral position if unconscious, once signs of life have been confirmed.
Note: Consideration of c-spine injury should take place during airway assessment and management. If injury is suspected, positioning and immobilising of the head in neutral alignment is indicated, but not at the expense of the airway.
Breathing
- Assess breathing for adequacy. Look, listen and feel for 5-10 seconds:
- Look:
- Equal rise and fall of chest wall
- Rate, regularity and effort of breathing
- Accessory muscle use
- Cyanosis (Blue tinge, commonly seen at the finger nails and lips)
- Tripod positioning
- Recessive breathing in paediatrics (sucking-in of chest wall) Listen:
- Abnormal noises associated with breathing (wheezes, crackles)
- Ability to talk in full sentences Feel:
- Rise and fall of chest
- Breath on cheek (unconscious patients only)
- Apply SpO2 monitoring if trained and authorised.
- Record dyspnoea score
- Correct any breathing problems encountered according to relevant CPGs or Skills (e.g. Ventilation).
- If patient is not breathing/not breathing normally, commence resuscitation.
Circulation
- Assess for bleeding and control any life threatening haemorrhage according to relevant skill/CPG.
- Palpate a pulse for 5 seconds. Note characteristics such as speed, regularity and strength.
Common pulse sites and situations include:- Carotid (unconscious patients, or conscious patients where radial pulse is difficult to locate)
- Brachial (infants)
- Radial (conscious adult patients)
- Apical (newborns)
- Assess capillary refill.
- Assess skin temperature and colour (useful in identifying shocked patients).
- Correct any life threatening circulatory problems according to relevant CPG.
- Where CPR is indicated and chest compression initiated, attach defibrillator as soon as possible to assist with restoration of circulation as per cardiac arrest CPG.
Disability
- Rapid assessment of brain function:
- Assess conscious level (AVPU/GCS)
- Assess pupil reaction to light (PERL)
- Assess neurological limb function (sensation, movement and strength)
- Perform BGL where patient is not fully alert and orientated to time, place and person
- Perform FAST test where stroke is suspected.
- If FAST positive, complete RACE evaluation
- Consider temperature where suspected of causing reduced conscious level
- Correct life threatening disability problems according to relevant CPG
Exposure & Evaluation
- Perform brief systematic head to toe evaluation: Expose:
- Potential injury/illness sites, manage according to relevant CPG
- Consider exposure to the elements, don’t leave exposed unnecessarily.
- Treatment/interventions provided
- Time critical status
Note: Any patient exhibiting significant primary survey problems is deemed time critical and requires urgent transportation to the nearest receiving hospital under Priority 1 conditions. Constant reassessment, life-saving interventions and a pre-alert/notification should be carried out en-route.
| Settings | |
|---|---|
| Extended Care: | |
| Colour assist: | |
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.