- This CPG is not intended to cover scenarios secondary to organic causes or to seek compliance with treatment of such. The primary strategy must be to address the underlying cause. This extends to circumstances such as CVA, trauma and post-resuscitation care. Consider SOC CSP consult.
- Active behaviour causing concern with a history of a recent crisis, emotional trauma, bizarre or abrupt changes in behaviour, suicidal ideation, alcohol/drug intoxication, and toxic exposure.
- ‘Agitated or Excited Delirium’, ‘Acute Behavioural Disturbance’ and ‘Drug Induced Psychosis’ are some alternative terms that might be used by other agencies to describe abnormal behaviours.
- Read more on Abnormal Behaviour in the Medical Library > Pathophysiology.
Administration of injectable sedatives under this CPG is limited to those with authority to practice per the Medications Schedule
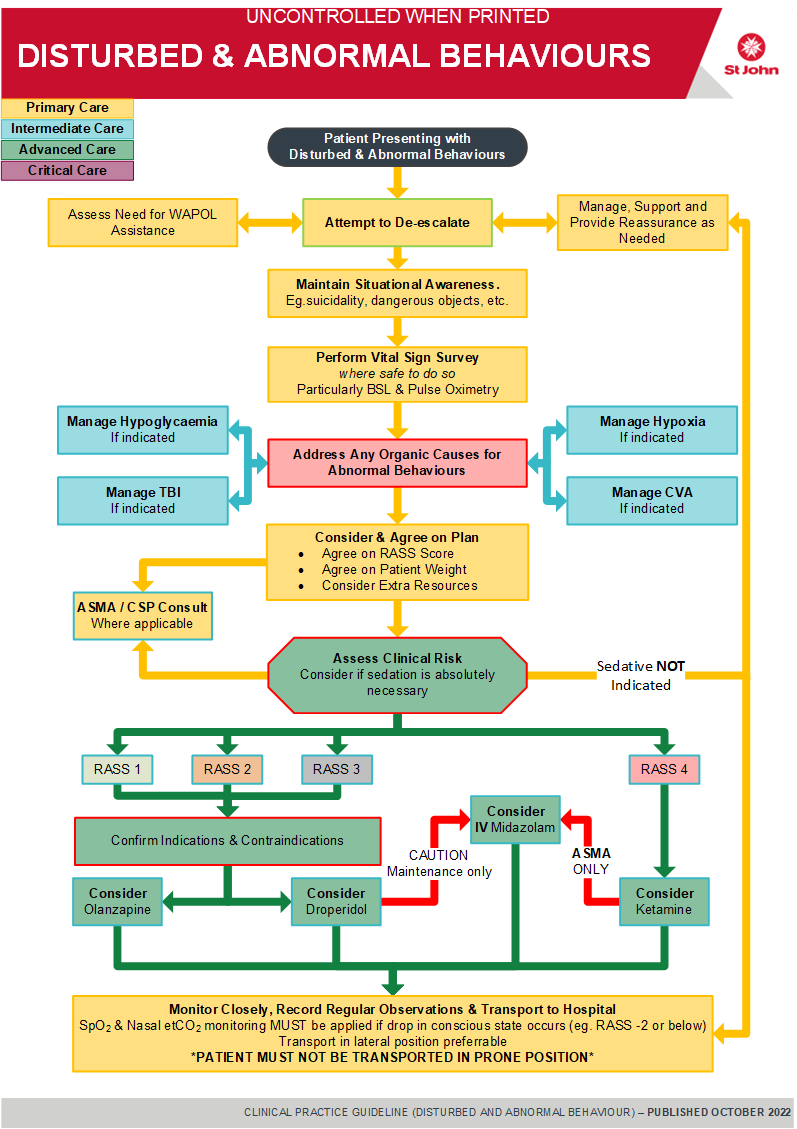
Applying a RASS score for the purposes of sedation should occur after meaningful de-escalation efforts
| Richmond Agitation Sedation Scale (RASS) | ||
|---|---|---|
| 4 | Severely agitated | Overtly combative, Violent, Immediate Danger or Threat |
| 3 | Very agitated | Aggressive behaviour, Unreasonable |
| 2 | Agitated | Frequent, Excessively Anxious, Loud outbursts |
| 1 | Restless | Mildly anxious, Non-Aggressive, Talkative |
| 0 | Alert & calm | |
| -1 | Drowsy | Sustained awakening to voice (>10s) |
| -2 | Light sedation | Awakens briefly to voice with eye contact (<10s) |
| -3 | Moderate sedation | Movement or eye opening to voice. No eye contact |
| -4 | Deep sedation | Movement or eye opening response to physical stimulus |
| -5 | Cannot be roused | Unresponsive to voice or physical stimulus |
- Address organic causes for behavioural presentations at all times- eg. CVA, TBI, Hypoxia, Hypoglycaemia, etc.
- Rarely, adrenal insufficiency patients may present with psychosis in acute crisis – history taking is important
- Be aware of personal safety at all times
- Only the police and Mental Health Transport Officers have legislated authority to apprehend persons in mental health circumstances (section 156 (1) Mental Health Act 2014). Patients transported under the Mental Health Act of 2014 must be in accordance with the Mental Health Transfer Clinical Practice Guideline and Interfacility Transfers procedure
- If the situation appears threatening, a show of force involving Police may be necessary before an attempt to restrain the patient is made. Consider your own safety and limitations. Use enough back-up to be confident and forthright
- If emergency treatment (sedation) is unnecessary, do as little as possible except to reassure while transporting. Be very aware of the patient’s “personal space”
- Sedation is HIGH RISK – must only be carried out after careful deliberation between officers and must not be based primarily at the request or influence of other agencies on scene (e.g. Police etc.)
- Positive RASS score does not automatically infer a need to sedate
- Age <16 years old – sedation should prompt a prior ASMA consult wherever practicable
- ETOH / Intoxication – apply caution
- Repeat & Maintenance doses – have a low threshold to consult with ASMA where repeat or maintenance doses are required
- Monitoring – SpO2 and EtCO2 monitoring must be applied whenever level of consciousness drops (~RASS -2 or below)
- Positioning – DO NOT transport in supine position (increases risk of laryngospasm from secretions) – transport in lateral position
- Airway & Breathing – monitor airway and breathing effort, including chest movement closely for signs of impairment. Prepare to support if required
- Restraint – Prone and/or handcuffed to rear carries excessive risk and MUST NOT occur. Physical restraint in any position that amplifies the risk of positional asphyxia, must be closely observed for signs of air hunger and hypoxia
- RASS scores must be agreed and documented
- Weight – Estimated weight must be agreed before administration of any weight based medicines. This must be documented
The final decision to sedate lies with the most senior clinician on scene
The guiding principle is that non-pharmacological techniques are first line and always preferable. If sedative medications are considered necessary, the most cautious approach should always be adopted.
- Primary Survey
- Before approaching, ensure safety of self, crewmate(s), bystanders and patient.
- If required, call for relevant assistance through the State Operations Centre, or urgent assistance (e.g. Police) via 000.
- Attempt to establish rapport through de-escalation and appropriate questioning and non-confrontational technique. Be aware of body language.
- De-escalation techniques should always be adopted (some RASS 3~4 cases may still respond favourably)
- Complete Vital Sign Survey, including BSL and Pulse Oximetry where safe to do so
- Repeat vital signs every 10 minutes, or 5 minutes if time critical
- Restrain only if essential to protect yourself and the patient using the minimum force necessary.
- Restraint may be verbal and / or physical depending on the individual circumstances.
- Section 243 of Criminal Code (7.4.2) states it is lawful for any person to use such force as is necessary in order to prevent a mentally impaired person from doing violence to any person or property.
- If appropriate, enquire sensitively about possible depression, helpless or hopeless feelings and thoughts of suicide.
- If patient expresses suicidal thoughts, do not leave patient alone.
- Carefully remove (have someone carefully remove) dangerous objects (e.g. knives, guns, pills) from the area.
- If appropriate, quietly question specifically about hallucinations or delusions and decide if patient is likely to act them out.
- Monitoring and transport principles as per Warnings above
- Do not allow patients to be handcuffed to the stretcher. Clearly document reasons if this cannot be achieved and the service number of the Police Officer.
- Consider additional support via SOC CSP and/or ASMA consult
Patients must never be transported prone
- Consider and address organic causes for disturbed behaviour as soon as practicable (including but not limited to head injury, hypoxia, hypoglycaemia and overdose, e.g. administer Glucose Oral Gel as indicated for hypoglycaemia)
- De-escalation techniques should always be adopted (some RASS 3~4 cases may still respond favourably)
- Consider Secondary and/or CNS Survey.
- Transport in a calm, quiet manner, monitor vital signs if you can without unduly agitating the patient.
- Refer to Mental Health Transfer Guidelines for patients being transferred under the Mental Health Act 2014.
- Consider and address organic causes for disturbed behaviour as soon as practicable (including but not limited to TBI, hypoxia, hypoglycaemia and overdose)
- De-escalation techniques should always be adopted as a first line (some RASS 3~4 cases may still respond favourably)
- Consider Secondary and/or CNS Survey
- Consider and agree whether sedation is appropriate and necessary. Have a high threshold (i.e. sedation should not be routine)
- Choice of agent requires sound judgement on a case basis and should normally align with a post de-escalation RASS score:
Note: IM Midazolam is not indicated for primary sedation. It is only to be used IV for maintenance of sedation - If sedation is agreed as unnecessary, continue de-escalation and reassurance as necessary.
- As per Advanced Care guidelines
- Police may be required to apprehend the patient or provide restraint in threatening situations.
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.