- Trauma to the spine may cause injuries involving the spinal cord, vertebrae or both.
- Spinal cord injury (SCI) can be identified when neurologic function above the injury is intact and function below the injury is absent or markedly diminished. Specific manifestations will depend on the exact level of injury.
- This guideline applies to the entire spinal column, including cervical, thoracic and lumbar spine.
Read the complete article; Spinal Cord Injury (SCI) in the Medical Library > Pathophysiology.
- Spinal assessment is a complex process that carries a high degree of clinical risk, thorough assessment is required to make an informed decision.
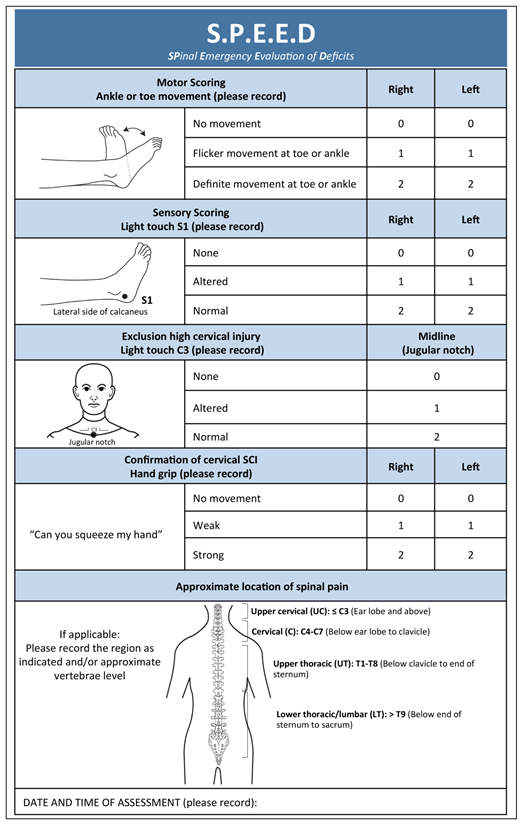
- Officers should consult the NEXUS Clinical Decision Rule (CDR) as indicated in the spinal assessment clinical skill and utilise the SPEED assessment tool
- NEXUS has been based on a large prospective observational study and can be used to identify patients at very low risk of cervical spine injury.
- The SPEED assessment tool should be used to identify patients with a high risk mechanism and who are at high-risk of spinal cord trauma and who will benefit from diversion to the State Trauma Centre.
- A SPEED score of ≤1 in any area indicates diversion to the state trauma centre when possible (PCH for paediatrics, RPH >14 years).
- Concerning children, no dedicated clinical decision tool for paediatric cervical spine trauma exists[1].
- Patients at the extremes of age (i.e. children and the elderly, or typically those ≥ 65 years of age) can be difficult to assess adequately. In both these patient groups, if the assessing clinician has any concern, immobilisation must be applied until full history and assessment (inclusive of imaging) prove spinal precautions could be discontinued.
It is important to assess and consider the entire spinal column, not only the cervical spine. If there is any thoracic or lumbar pain, consider against asking the patient to move themselves and instead lifting the patient for extrication, particularly in circumstances where additional support or resources are available
- SPEED assessment can indicate injuries along the entire spinal column and should be undertaken and used for all patients who cannot be cleared through NEXUS.
- C-Spine assessment is performed using clinical judgement and findings from examinations, the NEXUS Clinical Decision Rule can be used to aid this decision.
- Prior to clearance a thorough primary/secondary and SPEED assessment.
- Asses high risk factors that limit the ability to clear C spine
- Patients with no neurological deficit may self-extricate short distances (a few steps)
- Careful clinical judgment should be used, if self-extrication is likely to aggravate the injury then alternative methods of extrication should be used.
- Ensure a Lanyard is placed and education is given on self-splinting prior to self-extrication.
- Once on the stretcher apply head blocks and treat as though a spinal injury is present.
High risk factors include:
- Age: Older than 65 years
- Known pre-existing spinal conditions (e.g. ankylosing spondylitis, rheumatoid arthritis, spinal surgery, spinal stenosis etc.)
- Dangerous mechanism(s) of injury, including but not limited to:
- Fall: ≥ 1 meter OR 5 stairs
- High axial loading to the head (e.g. diving, rugby scrum, surfing etc.)
- Motor Vehicle Collision at high speed (≥ 60km/hr)
- Motor Vehicle Rollover
- Ejection from a vehicle
- Accidents involving motorised recreational vehicles (e.g. quad-bikes, ATV's, motorbikes, etc.)
- Bicycle collision
- Pedestrian/s struck by vehicle
- Abnormal neurological status
- Obvious or subtle numbness, tingling or strength deficit in peripheries which was not present prior to the incident/injury
- Abnormal neurological status which occurred prior to Ambulance arrival must be taken into account in conjunction with a SPEED assessment and consideration of a dangerous mechanism of injury. Document score and findings
In the absence of neurological signs, a co-operative pain free patient will generally not require a semi-rigid cervical collar. Patients that are able to self extricate without aggravation of their injury may be encouraged to take a few steps to the stretcher. Ensure a lanyard has been placed around the neck and they have received education about self splinting, to keep their head and neck as still as possible prior to movement. If the patient has or begins to experience neck pain, weakness in limbs or neurological signs during self-extrication attempts they should stop and the situation should be reassessed.
If a patient is unable to extricate themselves without assistance a spinal injury should be assumed. It is important that the patient moves themselves and is not assisted by the practitioner. If a patient getting up from the floor is going to aggravate their injury alternative methods such as a scoop stretcher should be used.
In the co-operative patient the following steps (spinal precautions) should be used:
- A lanyard should be placed around the patients neck prior to mobilistaion
- The patient should be provided with advice to keep their head and neck as still as possible and the reasons for this. The advice can be similar to the following:
"Evidence indicates no benefit to routine application of a Semi-Rigid collar in the absence of neurological symptoms. Because we cannot clear your neck we ask that you stay in a comfortable neutral position and avoid moving your head and neck as much as possible."
- Position patient supine, or semi-recumbent if more comfortable.
- Headblocks should be utilised to limit lateral movement and as a reminder (if appropriate for the patient)
An unco-operative patient who refuses to follow commands and advice, however, maintains capacity to do so will generally not tolerate a semi-rigid collar. Forcefully attempting to apply a semi-rigid collar may result in increased movement or agitation thus preventing the goal of the collar. Good clinical judgement is required with a careful analysis of risk vs. benefit. Organic causes of agitation and significant mechanisms of injury must be ruled out wherever practicable prior to adopting this approach.
General principles for consideration:
- Forceful placement of a semi-rigid collar is not recommended for the reasons above.
- The most feasible option is to continue to try manual stabilisation and repeatedly instruct the patient to remain still. The use of headblocks is encouraged and should be strongly considered. It is important that the head is not taped or strapped down.
- Ensure thorough documentation of the event and the situation
Follow guidance of medical staff.
In the absence of neurological signs, a co-operative pain free patient will generally not require a semi-rigid cervical collar. If a patient is able to self-extricate they should be encouraged to do so. The patient should also be instructed to keep their head and neck as still as possible. If the patient has or begins to experience neck pain, weakness in limbs or neurological signs during self-extrication attempts they should stop and the situation should be reassessed.
If a patient is unable to extricate themselves without assistance a spinal injury should be assumed unless able to be ruled out via the clinical decision rule. It is important that the patient moves themselves and is not manipulated by the practitioner.
In the co-operative patient the following steps (i.e. spinal precautions) should be considered:
- The patient should be provided with advice to keep their head and neck as still as possible and the reasons for this. The advice can be similar to the following:
"Evidence indicates no benefit to routine application of a Semi-Rigid collar in the absence of neurological symptoms. Because we cannot clear your neck we ask that you stay in a comfortable neutral position and avoid moving your head and neck as much as possible."
- Position patient supine, or semi-recumbent if more comfortable.
- Headblocks should be utilised to limit lateral movement and as a reminder (if appropriate for the patient) but are not routinely required.
- Ensure a warning lanyard is placed.
General Principles:
- If TBI is present and cervical injury cannot be ruled out, when possible position the patient to approximately 15 degrees to maximise cerebral drainage.
- Head block use is recommended to limit lateral movement.
- Avoid the triple airway manoeuvre if cervical injury is suspected.
- Once an advanced airway has been placed, the preferred option is to stabilise using appropriate padding, a warning lanyard and headblocks. A semi-rigid collar can be used, though is not recommended.
In situations where a semi-rigid Cervical Collar has been placed prior to ambulance arrival the following principles should be considered and followed:
- Engage in collegial handover and discussion around the reasons behind the decisions to place a cervical collar and St John Ambulance requirements to assess as per our Clinical Practice Guidelines
- Investigate if it is appropriate for the cervical spine to be cleared using the NEXUS clinical decision rule
- St John Ambulance Clinical Practice Guidelines should be followed if the patient cannot be cleared. This may mean replacing the collar with a different device.
- Appropriate discussion should take place prior to this undertaking.
- It is important to communicate with the patient the rationale behind the decisions that are being made. It is also important to emphasize that this decision is not a criticism of care that has been provided, rather a requirement of St John Ambulance guidelines. The initial care provider should also be involved in this discussion.
- If conflict with other providers arises, do not insist. Extricate and begin transport. Once underway further private discussion can be had with the patient, and the appropriate pathway of management can continue.
Employ spinal precautions if any of the following assessment findings are present, associated with trauma as defined above:
- SPEED Score ≤1 in any criteria (Neurological deficit)
- GCS <15
- GCS <15
- Spinal pain / tenderness / deformity
- Neurological deficit
- Significant mechanism of injury in conjunction with:
- Alcohol/drug intake
- Distracting injury
- Inability to communicate
- Primary Survey with C-Spine consideration
- Be aware of Trauma Management Principles
- Secondary / CNS Survey
A semi-rigid cervical collar should be placed if:
- The patient is unconscious with a mechanism of injury suggestive of possible cervical spine involvement OR
- The patient has neurological symptoms suggestive of spinal cord injury with a mechanism of injury suggestive of cervical spine involvement.
NOTE: Neurological symptoms suggestive of injury include (but are not limited to):
- Tingling in any extremity
- Numbness in any extremity
- Weakness of any limb/s
If a semi-rigid collar is placed, it is preferable to lift and extricate the patient via the use a of scoop stretcher. The patient should be rolled as little as possible. They should NOT be walked.
- If the patient is indicated per the assessment criteria above, utilise spinal immobilisation equipment, including:
- Cervical collar
- Head blocks
- Extrication board or orthopaedic (scoop) stretcher (and spider harness)
- Vacuum mattress
- Complete a SPEED assessment
- Administer anti-emetic as per CPG
- Consider pain relief
- Consider applying cardiac monitor if trained and authorised
- Monitor patient persistently, recording full observations every 10 minutes (or 5 minutes if time critical)
- Transport Priority 1 if patient time critical, pre-notifying receiving facility;
- Should a time critical patient be transported on an extrication board or scoop, full spinal immobilisation equipment should be used (cervical collar, head blocks and spider harness).
- The packaged patient must then be secured on the Ferno 50E stretcher.
- For inter-facility transfers, the Vacuum Mattress should ideally be utilised if available as per Clinical Skill.
A semi-rigid cervical collar should be placed if:
- The patient is unconscious with a mechanism of injury suggestive of possible cervical spine involvement OR
- The patient has neurological symptoms suggestive of spinal cord injury with a mechanism of injury suggestive of cervical spine involvement.
NOTE: Neurological symptoms suggestive of injury include (but are not limited to):
- Tingling in any extremity
- Numbness in any extremity
- Weakness of any limb/s
If a semi-rigid collar is placed, it is preferable to lift and extricate the patient via the use a of scoop stretcher. The patient should be rolled as little as possible. They should NOT be walked.
- If the patient is indicated per the assessment criteria above, utilise spinal immobilisation equipment, including:
- Cervical collar
- Head blocks
- Extrication board or orthopaedic (scoop) stretcher (and spider harness)
- Vacuum mattress
- Complete a SPEED assessment
- Administer anti-emetic as per CPG
- Consider pain relief
- Consider applying cardiac monitor if trained and authorised
- Monitor patient persistently, recording full observations every 10 minutes (or 5 minutes if time critical)
- Transport Priority 1 if patient time critical, pre-notifying receiving facility;
- Should a time critical patient be transported on an extrication board or scoop, full spinal immobilisation equipment should be used (cervical collar, head blocks and spider harness).
- The packaged patient must then be secured on the Ferno 50E stretcher.
- For inter-facility transfers, the Vacuum Mattress should ideally be utilised if available as per Clinical Skill.
- As per Advanced Care guidelines
- Patients should be padded appropriately to achieve their individual neutral spinal alignment (i.e. Most adult patients require a small amount of padding under the head, children may require padding under the torso, patients with increased thoracic kyphosis may require additional padding under the head at achieve the correct alignment).
- If a semi-rigid collar is indicated but unable to be applied (for example due to injury, patient habitus etc.) alternative options such as head blocks and/or in-line manual stabilisation should be considered and all considerations and decisions documented accordingly.
- Significant cervical spine injury due to hanging is uncommon. Routine cervical spine immobilisation is not required unless the body has fallen from a height greater to or equal to the height of the person.
- Cervical spine immobilisation is generally not required if there is an isolated penetrating injury to the neck (e.g. stabbing or gunshot). When multiple mechanisms of injury suggestive of spinal involvement are present immobilisation criteria should apply.
- When used the semi-rigid collar must be correctly sized and fitted to suit the patient. If this cannot be achieved the best approach should be reconsidered and alternative options such as head-blocks and/or manual in-line immobilisation should be considered. Patients may sit up on a slight incline (15 degrees) if they are experiencing difficulty breathing.
- Patients who are co-operative, ambulant and without neurological symptoms may self extricate short distances and coached to keep their head and neck as still as possible.
- Head blocks should be used to limit lateral movement if spinal precautions are indicated. Whenever possible, patients should be removed from scoop stretchers or extrication boards prior to transport due to risk of pressure injury.
The Royal Australian and New Zealand College of Radiologists. (2015). Paediatric Cervical Spine Trauma . Retrieved November 16, 2016, from RANZCR: http://www.ranzcr.edu.au/documents-download/3838-print-version-paediatric-cervical-spine
Connor, D., Porter, K., Bloch, M., & Greaves, I. (2013, December). Pre-hospital Spinal Immobilisation: An Initial Consensus Statement. Emergency Medicine, 30(12), 1067-1069.
Deasy, C., & Cameron, P. (2011). Routine application of cervical collars – What is the evidence? Injury, 841-842. doi:10.1016/j.injury.2011.06.191
Engsberg, J., J., S., Shurtleff, T., Eggars, J., Shafer, J., & Naunheim, R. (2013). Cervical Spine Motion During Extrication. The Journal of Emergency Medicine, 44, 122-127. doi:10.1016/j.jemermed.2012.02.082
Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. New England Journal of Medicine. 2000; 343(2): 94-9
Hood, N., & Considine, J. (2015). Spinal immobilisaton in pre-hospital and emergency care: A systematic review of the literature. Australasian Emergency Nursing Journal, 18, 118-137. doi:10.1016/j.aenj.2015.03.003
Kornhall DK, Jorgensen JJ, Brommeland T, et al. The Norwegian guidelines for the prehospital management of adult trauma patients with potential spinal injury. Scandinavian Journal of Trauma and Resuscitation Emergency Medicine. 2017;25:2.
Lee, M., McPhee, R., & Stringer, M. (2008). An evidence-based approach to human dermatomes. Clinical Anatomy, 21(5), 363-373. doi: 10.1002/ca.20636
Nikolić, S. & Živković, V. Cervical spine injuries in suicidal hanging without a long-drop—patterns and possible underlying mechanisms of injury: an autopsy study. Forensic Science, Medicine and Pathology (2014) 10: 193. doi:10.1007/s12024-014-9550-y
Oteir, A., Smith, K., Stoelwinder, J., Middleton, J., & Jennings, P. (2015). Should suspected cervical spinal cord injury be immobilised? :A systematic review. Injury, 46, 528-535. doi:10.1016/j.injury.2014.12.032
Paykin, G., O'Reilly, G., Ackland, H., & Mitra, B. (2017). The NEXUS criteria are insufficient to exclude cervical spine fractures in older blunt trauma patients. Injury, 48, 1020-1024. doi:10.1016/j.injury.2017.02.013
Stanton, D., Hardcastle, T., Muhlbauer, D., & van Zyl, D. (2017). Cervical collars and immobilisation: A South African best practice recommendation. African Journal of Emergency Medicine, 4-8. doi:10.1016/j.afjem.2017.01.007
Stiell IG, Wells GA, Vandemheen KL, Clement CM, Lesiuk H, De Maio VJ, et al. The Canadian C-Spine Rule for radiography in alert and stable trauma patients. JAMA. 2001; 286(15): 1841-8.
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.