
An urgent or emergency inter-hospital patient transfer occurs when the diagnostic or therapeutic needs of a patient are beyond the capacity of the initial hospital. The patient will require continued assessment and possibly treatment.
Non-emergency and/or general transfers that require an ambulance or Patient Transfer vehicle may be required for non-ambulatory patients or those that require continued assessment or care.
Prior to the transfer, crews should seek to understand the requirements of the case, e.g. what specific equipment is required to perform this transfer, are there Infection Prevention & Control requirements and/or concerns (e.g. communicable diseases), is there a specific crew configuration and/or medical escort requirements.
During the transfer, staff are required to reassess the patient appropriately, clearly document any changes in the patient’s condition or any interventions that have been undertaken (whether these are administered from St John or other medical staff).
A minimum of two sets of observations should be documented in this section.
- As a minimum requirement, Glasgow Coma Scale (GCS), Respiration Rate (RR), Pulse (HR) Blood Pressure (BP), Oxygen Saturation (SpO2) and pain scores. It should also include, where appropriate, any of the other parameters including pupils, ECG, end tidal Carbon Dioxide (etCO2), Blood Glucose Levels (BGL), temperature, dyspnoea and weight.
- Patient observations should be performed and documented every 20 minutes, and more frequently if clinically indicated. If this is not possible or is deemed clinically unnecessary the rationale should be documented.
- For PTS undertaking dual transfers, observations are taken at the point of pick up, and the second upon reaching the destination. Should there be any clinical deterioration of the patient, more frequent observations are also required, in addition to calling for Paramedic backup.
Inter-hospital patient transfers on an emergency basis occur when diagnostic or therapeutic needs of a patient are beyond the capacity of the initial hospital and are required on an emergent basis.
Non-emergency and/or general transfers that require an ambulance or Patient Transfer vehicle may be required for non-ambulatory patients or those that require continued assessment or care. Given the constraints present in the setting of a dual-stretcher vehicle, compliance with regards to the frequency of recorded of observations is limited to where safe and practicable.
Clinical Handover is essential in any transfer in order to provide continuity in patient care and should be conducted in accordance with the Clinical Handover Procedure.
In the context of interfactility transfers, the handover must follow the ISOBAR principles and be inclusive of (but not limited to):
- An adequate summary of the patient’s condition and level of acuity
- Current treatment
- Possible complications that could affect patient care in transit
- The transfer plan, as agreed by the treating team
This information should be conveyed verbally at the bedside and in a face to face fashion from the Doctor / Nurse in charge of the patient’s care and documented on the Interhospital Patient Transfer form (in ePCR or downloaded copy). Transfer paperwork (summary, lab work, x-rays, etc.) should be given to St John personnel prior to commencement of the transfer. The patient, family and or friends should be consulted regarding the transfer where appropriate.
If a nursing or medical escort is accompanying the patient, crew roles and responsibilities for the patient transfer should be discussed and be clear prior to commencement of the transfer.
In cases of an unexpected medical incident, unfamiliarity with vehicle layout and pre-hospital equipment by escorting medical teams poses a risk to patient safety and may hinder good patient outcomes. Where practicable, and to mitigate this risk, the attendant should be in the rear of the vehicle during the transfer. This may not be possible in specific circumstances, and should be included in the discussion regarding roles and responsibilities. The agreed plan should be documented.
It is essential that St John WA staff know the accepting doctor (or team) and the desired transport destination prior to departure.
The receiving physician should be contacted by the transferring physician, prior to transfer, with any updates and an expected estimated time of arrival.
The level of trained staff used to transfer a patient should be appropriate to the treatment necessary or anticipated during transfer. It may be appropriate for the hospital to send specifically trained personnel to accompany the patient. Crew mix requirements and role designations should be dictated by and commensurate with clinical transfer plan, patient acuity and the clinical needs of the patient. It is a requirement of St John WA that the most senior medical escort travel with patients in the patient compartment.
Team Roles
- St John WA
- Carrying out patient care and monitoring
- Documenting observations
- Operating the vehicle & SJWA equipment
- Nurse
- Managing Intravenous infusions
- Assisting with patient care and monitoring
- Doctor
- Overseeing patient care
The Doctor is the team leader and final decision maker. All opinions and concerns by all team members need to be freely expressed at all times.
Graded Assertiveness
Bring to attention
e.g. "The oxygen saturations are decreasing "
Enquire
e.g. "You're not going to cannulate that fractured arm, are you?"
Clarify
e.g. "I feel uncomfortable about this; please explain what you are doing."
In critical or dangerous situations, demand a response or take control
e.g. "LISTEN!" or "Stop – you must listen to me."
Staff must be comfortable that they have sufficient information to accept responsibility of a patient with ongoing medication administration. Instructions for oral, IM or IV maintenance should be provided for the St John WA staff.
Written instructions MUST be given on the Special Medication Authority section of the checklist for any medication not covered in St John WA Medication Protocols. Direction should also be sought from the transferring hospital or CSPSOC with regards to the disposal requirements of medications not covered by SJWA Medication Protocols.
Electronic infusion devices may be managed by St John WA staff without the need for an escort, however the following information is required:
- A direct contact number for attending doctor if more information becomes necessary
- A tutorial is given on how to adjust rates, turn the alarm off or stop the infusion as required
- Familiarity with Clinical Skill – IV Pumps
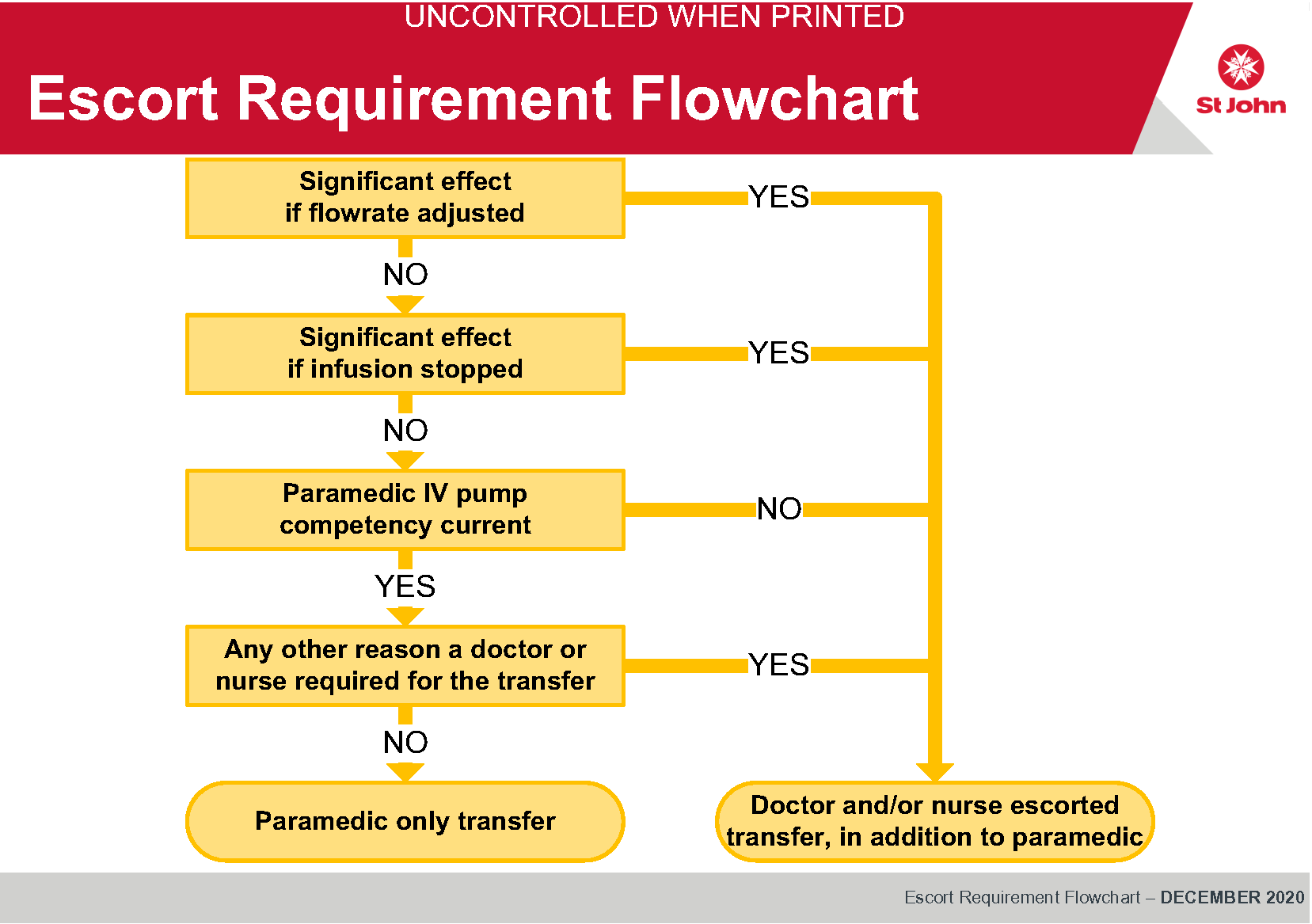
If presented with an IV infusion, the key questions to address are:
- What medication?
- What would be the effect if the flow rate was adjusted?
- What would be the effect if during the journey it stopped?
- If the effects of stopping the infusion or altering the infusion rate are life-threatening or severe, a suitable escort is required.
Key Terms & Links
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.