- To decompress a suspected tension pneumothorax
- Simple Pneumothorax
- < 12 years
- The potential for exposure to blood and body fluids is HIGH. All precautions that serve to minimise risk to the clinician and the patient are to be applied.
- Clinicians should be double-gloved with sterile gloves on the outside.
- In traumatic cardiac arrest, finger thoracostomy should be performed bilaterally, starting on the side with the suspected tension pneumothorax.
- If patient is conscious, perform procedure on affected side only.
- There is significant risk of injury to the clinician in case of chest trauma where rib fractures may occur. Extreme caution to be taken when inserting finger into the tract.
- Incorrect placement may result in life threatening injuries to the heart, lung or surrounding vessels.
- All relevant infection control methods are to be utilized.
- Prepare equipment required:
- Underpad / bluey
- Sterile kidney dish
- Necessary PPE including sterile gloves; double glove
- Disposable Scalpel
- Face shield for clinician and assistant
- Povidone-Iodine Swabs
- Ferno Sam Chest Seal
- Sterile gauze
- Haemostatic Forceps
- Consider appropriate analgesia for the conscious patient:
Patient positioning
- The patient should ideally be positioned supine, alternatively in the most comfortable position.
- The arm on the affected side should be abducted and externally rotated, simulating a position in which the palm of the hand is behind the patient’s head.
- An underpad / bluey should be placed under the side where the finger thoracostomy is to take place to absorb draining bodily fluids.
Patient preparation
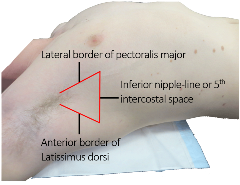
- Position the patient as described above, identifying the ‘triangle of safety’ as shown[1]
- Identify the fifth intercostal and the midaxillary line on affected side:
- The skin incision is made in between the midaxillary and anterior axillary lines over a rib that is below the intercostal level selected
- Shave excessive hair and clean a wide area of the chest wall area with Povidone-Iodine Swab[2]
- Administer analgesia (conscious patient):
- Use a needle to inject 50-100mg (5-10mL) of the local anaesthetic solution into the intercostal muscle superior to the expected initial incision.
- Administer ketamine for procedural sedation (unless contraindicated or patient unconscious)
Performing the procedure
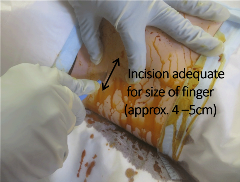
- Use the scalpel to make a horizontal skin incision adequate size for the insertion of finger (approximately 4 – 5cm long) overlying the rib that is below the desired intercostal level of entry. The skin incision should be in the same direction as the rib itself[3]
- Dispose of the used scalpel immediately into the sterile kidney dish
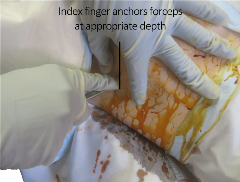
- Use the haemostatic forceps to bluntly dissect a tract in the intercostal space.
- Anchoring the forceps with your index finger at a depth estimated to enter the pleural space; used the closed forceps to bluntly dissect a tract through the intercostal muscles and parietal pleura and enter into the pleural space as shown[4].
- This manoeuvre may require some force and should be done in a controlled fashion so the instrument does not enter too far into the chest, which could injure the lung or diaphragm. Use a twisting motion of the tip of the closed forceps to open and enter the pleural space. The "give" of the parietal pleura indicates access to the pleural space.
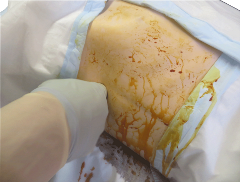
- Remove the forceps.
- Insert your full gloved finger into the space and perform a finger sweep to ensure access to the pleural space[5].
- Assess for the release of air and/or blood. You may also be able to palpate the lung parenchyma and detect lung inflation/deflation, especially if patient is receiving positive pressure ventilation
(i.e. intubated). - Apply the seal over the incision and ensure seal adequately placed[6].
- Reassess continuously for the redevelopment of a tension pneumothorax. Be prepared to repeat steps 7 – 10 if required.
- Reassess continuously for the redevelopment of a tension pneumothorax. Be prepared to repeat steps 7 – 10 if required.
| Settings | |
|---|---|
| Extended Care: | |
| Colour assist: | |
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.