Effective and timely airway management is a priority for sick and injured patients. The benefit and conduct of pre-hospital emergency anaesthesia (PHEA) and advanced airway management remains controversial but there are a proportion of critically ill and injured patients who require urgent advanced airway management prior to hospital arrival1 and the evidence shows us the benefits of this procedure when carried out with the appropriate training, education, robust competency framework and overarching clinical governance. It is a challenging procedure, and repeated attempts endotracheal intubation is associated with increased morbidity and mortality. It follows that this is a skill that should only be performed by appropriately trained and competent practitioners working in a properly structured prehospital system. This includes the mandatory use of standardised RSI checklists which have been proven to reduce cognitive load, eliminate individual practitioner variability, reduce error, and confirm availability of equipment, doses of drugs and failed intubation management plans.
Standards of practice and monitoring should be similar to those recommended for in-hospital anaesthesia.
Emergency anaesthesia is carried out to facilitate control of the airway and ventilation of critically ill patients. There are four broad indications for the procedure:
- Failure of airway maintenance or protection
- Failure of oxygenation or ventilation
- Predicated clinical course/humanitarian reasons
- To facilitate safe transportation
The decision to perform prehospital anaesthesia should be based on a thorough consideration of the RISKS vs BENEFITS to the individual patient. This should take into account:
- Estimated transfer time to definitive care
- Clinical indications for performing prehospital anaesthesia
- Skill set available
- Relevant patient comorbidities
- Alternatives
| Factors in favour of on-scene intubation | Factors against on-scene intubation |
|---|---|
|
|
Time pressures in the pre-hospital environment mean practitioners rarely have the luxury of performing a comprehensive airway assessment. Tools such as the Aintree six-step approach to potentially difficult airways highlight the following important questions to ask prior to setting up for an RSI/DSI:
- How much time do I have?
- What access to the airway is available?
- How compromised is the airway?
- What fascial planes are involved?
- What management plan best fits the circumstances?
- Could I make the situation worse? If so, how?
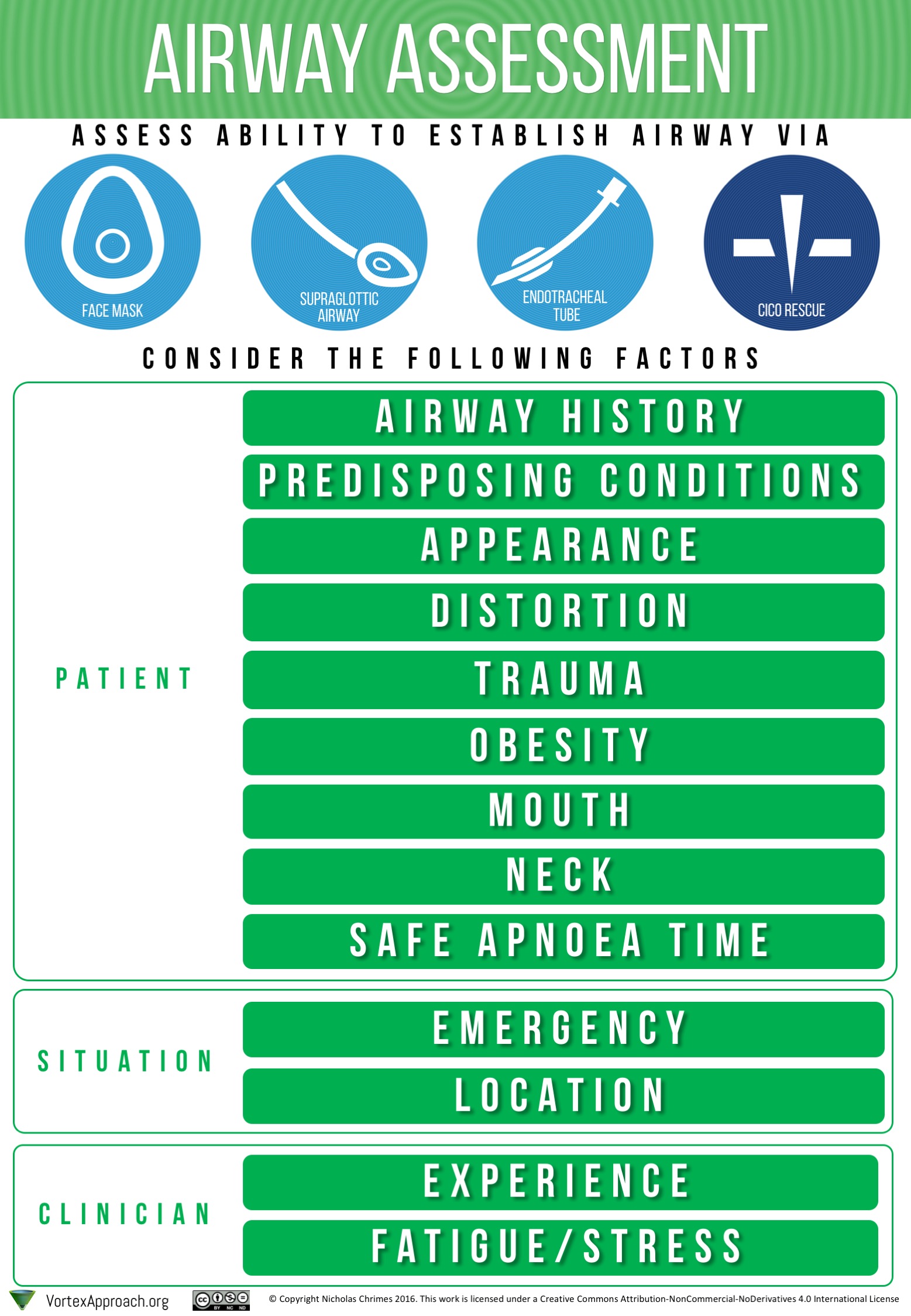
Additionally, cognitive aids such as the Airway Assessment chart displayed, take from The Vortex approach, provide a simple way of approaching an airway assessment.
- Always use the RSI checklist to facilitate set up and preparation
- Establish bilateral IV/IO access
- Establish monitoring (SpO2, ETCO2, NIBP – cycling every 3 minutes, ECG)
- Assemble dump kit
- Prepare pre-drawn RSI medication and doses
- VAPORS assessment
- Establish failed intubation plan and equipment
- Optimise patient environment
- Upright position if possible or 30 degree tilt
- OOPS ("Oxygen On, Pull mandible forward, Sit upright if possible")
- C-spine conisiderations
- Check IV/IO access patent
- Prehydration with fluid +/- blood
- Optimise haemodynamics
- Consider inotropic support
Preoxygenation is vital for safe prehospital anaesthesia and should proceed through the entire preparation phase. A variation to RSI is that of DSI or Delayed Sequence Induction, which is generally described as the process of pre-oxygenation with sedation in advance of paralysis.
The table below illustrates a guide for the most appropriate form of preoxygenation for different patient groups as per their risk category:
Table 1: Risk categorization of patients during preoxygenation
Risk Category Based on pulse oximetry whilst receiving high flow oxygen | Preoxygenation Period (3 minutes) | Onset of muscle relaxation (~ 60 seconds) | Apnoeic period (Variable duration dependent on airway difficulty, ideally <30 seconds) |
|---|---|---|---|
| Low risk (SpO2 96-100%) |
|
|
|
| High risk (SpO2 91-95%) |
|
|
|
| HYPOXAEMIC (SpO2 <91%) |
|
|
|
- Consider fluid challenge (blood or crystalloid) and/or inoptropic support for haemodynamically compromised.
- Fentanyl
- 2-3mcg/kg IV / IO
- Indicated in raised ICP and cardiovascular disease (e.g. great vessel rupture/dissection, aneurysmal disease, IHD)
- Helps decreases catecholamine discharge secondary to intubation, thus decreasing risks associated with increases in blood pressure in patients with cardiovascular disease, aortic dissections etc.
- Ketamine
- 1-2mg/kg IV / IO
- Indicated for any RSI.
- Use cautiously with active cardiovascular injury (MI) or heart failure.
- Ketamine exerts complex pharmacological actions including inhibition of biogenic amine uptake, binding to opioid receptors. Synergistic effect with opioids to produce desired sedation and analgesia.
- Apnea is a rare side effect of ketamine.
- Midazolam
- 0.03 mg/kg
- Indicated for patients with ketamine sensitivity or contraindications to same. (Thyroid replacement therapy or known allergy.)
- Use cautiously due to vasodilator and respiratory depression.
Pre-drawn RSI drugs in standardised concentrations have been introduced as a means of reducing drug related errors.
- Fentanyl: 500mcg in 20ml (25mcg/ml)
- Induction dose of 1-3mcg/kg
- Ketamine: 200mg/20ml (10mg/ml)
- Induction dose of 1-2mg/kg
- Rocuronium: 200mg in 20ml (10mg/ml)
- Induction dose of 1.2-2mg/kg
- Consider BURP/bimanual laryngoscopy to facilitate passing the tube
- Maintain sight of tube passing through cords and position appropriately
- Confirm placement by visualization, auscultation, etCO2 (6 non diminishing wave forms)
- Use of RSI post intubation checklist
- Note position of ETT at teeth
- Secure tube (consider tape in head injured/children)
- Secure all lines/equipment
- Appropriate sedation and paralysis
- Establish appropriate ventilator settings for patient condition
- Check VBG to titrate settings to clinical condition
- Use of Pre-scene departure checklist for packaging and final checks
Table of initial ventilator settings and tips for titrating
| Parameter | Normal lungs | ARDS/ALI | Asthma/COPD | Metabolic Acidosis | Head Injury | Severe obesity | |
|---|---|---|---|---|---|---|---|
| Aim | Lung protective strategy | Recruitment, shunt retention, avoid atelectic trauma, achieve adequate oxygenation | Oxygenation, adequate exhalation avoiding breath stacking and volutrauma | Ensure adequate respiratory rate to maintain and even improve compensation for metabolic acidosis | Avoid reduced venous return by avoiding high intrathoracic pressures | Avoid atelectasis and shunting due to obesity | |
| Position | 20-30 degree head up unless hypotensive and reduced cerebral perfusion a concern | ||||||
| Mode | VC (SIMV) | VC (SIMV) | PC (APRV equiv.) | VC (SIMV) | VC (SIMV) | VC (SIMV) | VC (SIMV) |
| VT (mL/kg) | 8 | 6 | monitor | 5-8 | 8-10 | 6-8 | 8-10 |
| Respiratory rate | 14 | 14 | 14 | 8-10 | 20-30 | 16 | 14 |
| I:E Ratio | 1:2 | 2:1 | 2-4:1 | 1:4-1:5 | 1:1-1:2 | 1:2 | 1:1-1:2 |
| Pinsp (cmH2O) | - | - | 25-30 | - | - | - | - |
| PEEP (cmH2O) | 5 | 10-15 | 10-15 |
| 5 | 5 | 10-15 |
| FiO2 | Start at 100% and rapidly titrate down, ideally achieving FiO2 0.4. Avoid significant hyperoxia. Aim for oxygen saturations > 95%; pO2 >80. Aim Pplat <30. | ||||||
| Other | Adjust parameters to ensure O2 and CO2 within normal limits | Watch pressures; may need to lower Vt and accept higher CO2. Titrate FiO2 and PEEP | Minimise derecruitment | Minimise derecruitment, i.e. minimise suctioning and disconnection. Consider recruitment manoeuvres | Watch for breath stacking and volutramua or barotrauma. Consider permissive hypercapnia. pH >7.15. May need to accept higher peak pressures in asthmatics. Aim Pplat <30 | Avoid high PEEP if possible. Aim PCO2 35-40. Tape rather than tie ETT to avoid impeding jugular vein flow. | Minimise decruitment, i.e. minimise suctioning and disconnections |
| Settings | |
|---|---|
| Extended Care: | |
| Colour assist: | |
Christine M. Groth, Nicole M. Acquisto, Tina Khadem. Current practices and safety of medication use during rapid sequence intubation,Journal of Critical Care,Volume 45,2018,Pages 65-70,ISSN 0883-9441,https://doi.org/10.1016/j.jcrc.2018.01.017.
Brandon G. Santoni, Ph.D. ; Bradley J. Hindman, M.D. ; Christian M. Puttlitz, Ph.D. ; Julie B. Weeks, M.P.T. ; Nathaniel Johnson, B.S. ; Mazen A. Maktabi, M.D. ; Michael M. Todd, M.D.Manual In-line Stabilization Increases Pressures Applied by the Laryngoscope Blade during Direct Laryngoscopy and Orotracheal Intubation. Anesthesiology January 2009, Vol. 110, 24–31.https://doi.org/10.1097/ALN.0b013e318190b556
Jeffrey L. Jarvis, MD. 2016. Using DSI to Prevent RSI from Becoming RSD (Rapidly Sequenced Death). Williamson County EMS. http://txemsa.com/using-dsi-to-prevent-rsi-from-becoming-rsd
Manoach, Seth & Paladino, Lorenzo. (2007). Manual In-Line Stabilization for Acute Airway Management of Suspected Cervical Spine Injury: Historical Review and Current Questions. Annals of emergency medicine. 50. 236-45. 10.1016/j.annemergmed.2007.01.009.
Robitaille A, Williams SR, Tremblay MH, Guilbert F, Thériault M, Drolet P. Cervical spine motion during tracheal intubation with manual in-line stabilization: direct laryngoscopy versus GlideScope videolaryngoscopy. Anesth Analg. 2008 Mar;106(3):935-41, table of contents. doi: 10.1213/ane.0b013e318161769e. PMID: 18292443.
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.