Glossary of Terms:
- PIVC: Peripherally inserted intravenous catheter
- DIVAS: Difficult intravenous access score
- PIVAS: Peripheral intravenous catheter assessment score
- Administration of intravenous fluids where oral intake is unavailable or unsuitable
- Administration of intravenous medications where other routes are inappropriate or unsuitable
- Unstable or deteriorating patients
- Directly over or distal to:
- Burns
- Cellulitis
- Infection
- Injury
- Frail or immunocompromised patients unless clinically warranted
- More than 2 attempts by appropriately trained and skilled clinician
- More than 1 attempt of vascular access (IV/IO) in traumatic cardiac arrest
Key Aseptic Terms for PIVC
- Key Sites:
- Insertion site of PIVC
- Key Parts:
- Cannula
- Syringe
- Tegaderm
- Blood Collection Vacutainer
- Cleaning Swab
- Bung
- Consider if PIVC is necessary, has benefits that outweigh the risk to the patient, or if there are any alternatives available.
- Insertion of PIVC's should be based on minimising patient discomfort, whilst utilising the smallest appropriate sized cannula to provide ease of insertion and therapeutic benefit.
- Ensure all principles of aseptic technique are adhered to. If aseptic technique is not possible (for example, time critical patients) then document on ePCR that PIVC was not inserted aseptically and hand over to receiving facility.
- Consider patient history regarding PIVC insertion, particularly history of requiring ultrasound guided insertion or history of infection from PIVC's.
- Utilise Difficult IntraVenous Access Score (DIVAS) to assist with identifying difficult or high risk patients.
- In Acute Coronary Syndrome patients, preference is for PIVC insertion into the LEFT arm in anticipation of percutaneous coronary intervention/Cath lab.
- Utilise and document Peripheral Intravenous Assessment Score (PIVAS) as required
- Avoid limbs with previous lymph node clearance due to increased risk of lymphoedema.
- Only use sites distal to fistulas as a last resort.
- If patient has chlorhexidine sensitivity/allergy, use 10% povidone-iodine swab.
- J-LOOP EXTENSION SET IS NOT TO BE USED FOR MAJOR TRAUMA OR RAPID FLUID RESUSCITATION
| Location guide | ||
|---|---|---|
| Location | Benefits | Negatives |
| Metacarpal and Forearm | Easily accessible Self-splinting | Metacarpal may have increased risk of phlebitis and trauma if not appropriately secured |
| Ante-cubital fossa | Suitable for large bore cannulas – 16g to 18g. | Increased risk of infection Increased likelihood of occlusion Poor accessibility - particularly in OHCA Increased risk of PIVC dislodgement |
| Ankle and Feet | Only used as a last resort | Increased chance of infection |
| Sizing guide | |||
|---|---|---|---|
| Size | Suitable for | Flow rate (up to) | Example procedures |
| 14g | CCP USE ONLY: Rapid volume replacement | 360mL/min | Major Trauma |
| 16g | Volume replacement | 220mL/min | Trauma, PPH/Obstetric |
| 18g | Fluid administration | 110mL/min | ACS, Sepsis |
| 20g | Fluid and medication administration | 63mL/min | ACS, dehydration, Sepsis |
| 22g | Difficult access/paediatric patients/small target vein | 38mL/min | Medication/fluid administration |
| 24g | Difficult access/paediatric patients/small target vein | 24mL/min | Medication administration |
NOTE: Flow rates based on JELCO VIAVALVE Safety IV catheters without utilising a bung. Maximum flow rate using a bung is up to 208ml/min.
Difficult Intravenous Access Score (DIVAS)
The difficult intravenous access score is a diagnostic tool intended to help identify patients who are considered to have difficulty with gaining access with a peripherally inserted intravenous catheter. DIVAS has been found to improve first attempt success, and helps to identify the required seniority for a cannulation attempt. The table below provides a cumulative score from 5 to 15, with 5 being considered very difficult access and 15 not having any identified difficult intravenous access factors.| DIVAS Score | Intended Action / Guidance |
|---|---|
| 5 – 8 (Poor) | Patient considered to have difficult IV access. PIVC should only be attempted if critical or access is crucial. Only to be performed by the senior clinician on scene. |
| 9 – 11 (Moderate) | Patient may have some difficulty in gaining IV access. Only to be performed by the senior clinician. |
| 12 – 15 (Excellent) | Minimal factors identified for patient to have difficult IV access, can be performed by appropriately trained staff. |
| DIVAS Categories | |||
|---|---|---|---|
| Categories | 3 | 2 | 1 |
| Number of Veins Visible/Palpable | 4-5 | 2-3 | 0-1 |
| Skin Condition | Excellent | Moderate | Poor |
| Skin Turgor | Excellent | Moderate | Poor |
| Vein Mobility | Low | Moderate | High |
| Hx of ultrasound guided PIVC insertion | No | Once | Regularly |
| DIVAS Criteria | |||
|---|---|---|---|
| Criteria | Excellent | Moderate | Poor |
| Veins Visible | Number of veins able to be seen/palpated on application of a tourniquet | ||
| Skin Condition | Skin has good health:
Veins are:
|
Skin has reasonable health:
Veins are:
|
Skin is in poor health:
Veins are:
|
| Skin Turgor | Skin immediately returns to normal position | Delay in skin returning to normal however skin returns to normal | Skin does not fully return to normal position despite delay |
| Vein Mobility | Low:
| Moderate:
| High:
|
Preparation:
Patient:
- Explain procedure to patient and gain consent where required
Equipment:
- appropriately sized cannula, utilise location and size guide as required
- Pre-drawn syringe of Sodium Chloride 0.9% if available. If not, draw up 10mL of Sodium Chloride 0.9% into a 10mL syringe
- 2 x 2% CHG 70% alcohol swab (10% povidone – iodine swab if patient allergic)
- Needle free valve (bung) OR J-loop extension kit
- Single patient use tourniquet
- Transparent IV dressing (Tegaderm)
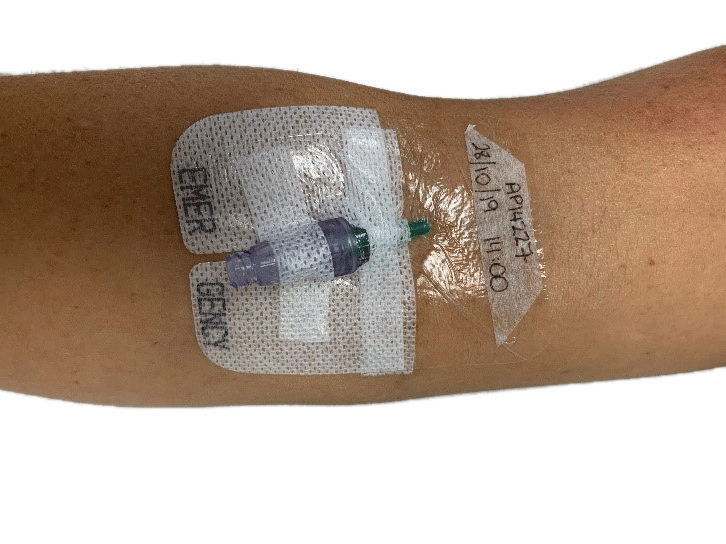
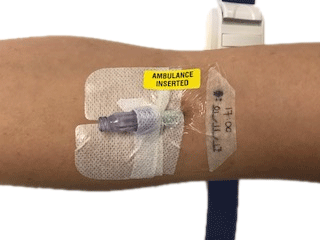
- “Ambulance inserted” sticker (if EMERGENCY printed Tegaderm unavailable)
- Sharps container
- Do not pre-open equipment packets: Only open the equipment when about to perform the skill.
Site:
- Select appropriate site, clean with cleaning wipe if visibly soiled. Shave site if required.
- Utilise location guide, sizing guide and DIVAS tools.
- Utilise patient positioning to ensure best access to site.
- Apply tourniquet proximal to insertion site.
- Extended Care
- Difficult access: Consider BOA Constricting Band
- Perform hand hygiene, don fresh gloves if potential of further exposure to blood or body fluid during cleaning.
- Thoroughly clean the site with the appropriate antiseptic swab by wiping the swab in a cross-hatch manner across the patients skin for 30 seconds and allow to air dry. Cross-hatch can be achieved by wiping the site in an up and down method for 15 seconds, then using a fresh wipe, wipe the site in a side to side method for 15 seconds (if patient is time critical document if unable to wait for 30 seconds).
- Do not touch or palpate the site again.
Cannula insertion, use and removal
Insert the cannula
- Perform Hand Hygiene and don fresh gloves
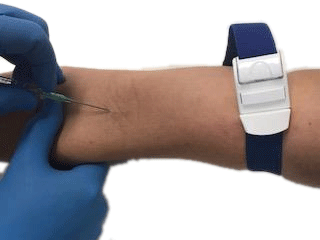
- Stabilise vein and insert cannula 30° bevel up
- Observe for flashback into the chamber
- Reduce the angle of the cannula and slightly advance the cannula and needle to ensure entry of catheter into vein
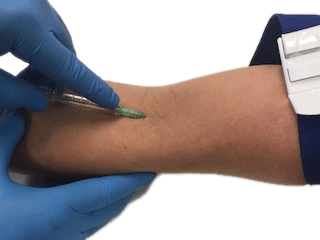
- Slide cannula over needle until you hear a ‘click’, dispose in sharps container
- If obtaining blood sample, refer to CPG clinical skill
- Release tourniquet
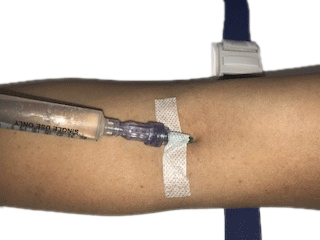
- If using bung: attach needle free valve (bung) and gently flush with 5-10mL of normal saline 0.9%
- If using J-Loop extension set: Prime J-loop with normal saline 0.9% IF NOT OBTAINING PRE-HOSPITAL BLOOD SAMPLE.
- Attach J-Loop extension set.
- Gently flush J-Loop with 5-10mL of normal saline 0.9%
- Secure cannula with transparent dressing, notating time and date on to label. Note: Do not place the dressing on to another surface prior to placing on patient skin.
- If using cohesive gauze, attempt to have insertion site visible/easily accessible.
- In case of arterial cannulation
- Identify potential arterial cannulation:
- Look for bright red, pulsatile backflow into syringe when flushing
- Upon identifying arterial cannulation, or if concerned cannulation is arterial:
- Do not administer any medications or use the cannula
- Leave cannula in place
- Cover site with gauze, label and secure gauze
- Alert staff on handover of arterial cannulation
- Identify potential arterial cannulation:
Using the cannula
- Prior to administration of medications, fluids or flushes, the bung or J-Loop port requires preparation:
- Using appropriate cleaning swab, wipe and clean the bung/port and syringe for 15 seconds
- Allow to air dry
- Administer medication, fluids or flush.
- If utilising pre-drawn syringe of Sodium Chloride 0.9% then cleaning of syringe not required unless contaminated/cap has been removed prior to flush.
- If utilising Sodium Chloride 0.9% drawn into a 10mL syringe, then cleaning of the tip of the syringe with an alcohol wipe will be required.
- It is recommended to flush the cannula every 4 hours to ensure patency.
- When using the cannula, perform a PIVAS assessment to ensure no signs of infection.
Removal of the cannula
- Explain procedure to patient and gain consent
- Perform hand hygiene
- Remove adherent dressing. Be mindful of frail/elderly patients at risk of skin tears when removing adhesive dressing.
- Utilising aseptic technique, place sterile dressing over insertion site of cannula
- In one continuous motion, gently pull the cannula until completely removed.
- Prior to disposal of cannula, inspect to ensure cannula is intact.
- Dispose of PIVC immediately into sharps container (unless otherwise directed by hospital staff)
- Utilising aseptic technique, place IV pressure dressing (dot) on to site, observe for bleeding.
Peripherally Inserted Vascular Access Score (PIVAS)
- Upon handover of patient with PIVC inserted
- Every four hours if patient has PIVC inserted
- Post administration of IV medications or fluids.
- Patient complains of pain or discomfort from site of PIVC.
| PIVAS Score | ||
|---|---|---|
| Signs and Symptoms | Action required | |
| PIVAS 0 Healthy PIVC site |
| No action needed, replace dressing using aseptic if not clean or dry, or if dressing is no longer secure. |
| PIVAS 1 Low risk | ONE of the following are present at site of PIVC:
|
|
| PIVAS 2 Moderate Risk | TWO of the following are present at the site of the PIVC:
|
|
- PIVC flushes easily, administer medications as per guidelines
- PIVAS Score is 0
- Pain, discomfort or difficulty in administering intravenous fluids or medications.
- PIVAS score is 1 or above
Potential complications of attempting intravenous access:
- Insertion and use of a PIVC can pose a significant infection risk to patients.
- Arterial puncture
- Cannula shear
- Extravasation
- Haematoma or haemorrhage
- Nerve damage
- Phlebitis
- Air embolus
- Vasovagal syncope
| Settings | |
|---|---|
| Extended Care: | |
| Colour assist: | |
Clare S, Rowley S. Best practice skin antisepsis for insertion of peripheral catheters. British Journal of Nursing. 2021 Jan 14;30(1):8-14.
Carr PJ, Rippey JC, Cooke ML, Bharat C, Murray K, Higgins NS, Foale A, Rickard CM. Development of a clinical prediction rule to improve peripheral intravenous cannulae first attempt success in the emergency department and reduce post insertion failure rates: the Vascular Access Decisions in the Emergency Room (VADER) study protocol. BMJ open. 2016 Feb 1;6(2):e009196
van Loon FH, Puijn LA, Houterman S, Bouwman AR. Development of the A-DIVA scale:: a clinical predictive scale to identify difficult intravenous access in adult patients based on clinical observations. Medicine. 2016 Apr;95(16).
Barr N, Mason M, Clegg L, Randall F. Maintaining asepsis in paramedicine: a Delphi study: Asepsis in paramedicine. Australasian Journal of Paramedicine. 2022 Apr 13;19.
Australian Commission on Safety and Quality in Healthcare. NSQHS Standards Implementation guide for Action 3.11 Aseptic Technique. December 2022. https://www.safetyandquality.gov.au/sites/default/files/2022-01/nsqhs_standards_implementation_guide_for_action_3.11_aseptic_technqieu_-_december_2021.pdf
Document Control
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.