
Definitions
- DATP: Dual Antiplatelet Therapy
- EF: Ejection fraction
- LAD: Left anterior descending artery
- LCx: Left circumflex artery
- OHCA: Out of hospital Cardiac Arrest
- RCA: Right coronary artery
- VF: Ventricular fibrillation
Case Study
We received a triple-zero call for a 65 year old male from his wife, stating that he had suffered a seizure but was now conscious and breathing. The call was dispatched as Priority 2. Upon arrival, the patients’ wife stated that he had lost consciousness whilst sitting in a chair; she pulled him down to the ground, his eyes rolled back and she saw him foaming at the mouth. She commenced CPR thinking that he had gone into cardiac arrest, but she stopped shortly afterwards as he regained consciousness.
We were led into the living room where the patient was found lying supine with his head on a pillow and we commenced our assessment. Clinically the patient presented as relatively unremarkable and the primary survey revealed nothing of immediate concern; the patient was alert (though cool peripherally), he had a delayed capillary refill of 3 seconds and a weak radial pulse.
Initial observations:
- Respiratory rate: 16/min
- Oxygen saturations: 99% RA
- Heart rate: 60/min
- Blood pressure: 130/70
- GCS: 15
- BGL: 6.8
- Temperature: 36.3°
Upon further questioning it was identified the patient had suffered a sudden VF arrest 6 weeks prior and had since made a complete recovery. He was now on dual antiplatelet therapy (DATP) and ACE inhibitors. The patient was otherwise fit and well, normal BMI, non-smoker and consumed alcohol socially. His only complaint was feeling mildly dizzy and lightheaded; he denied any pain, nausea or shortness of breath.
Previous Medical History
- Cardiac stent of RCA and LCx
- OHCA (VF)
Medications
- Ramipril
- Aspirin
- Clopidogrel
- Metoprolol
- Atorvastatin
Notes
- Echocardiogram unremarkable. EF 70%, all valves appear healthy
- Angiogram mild stenosis LAD
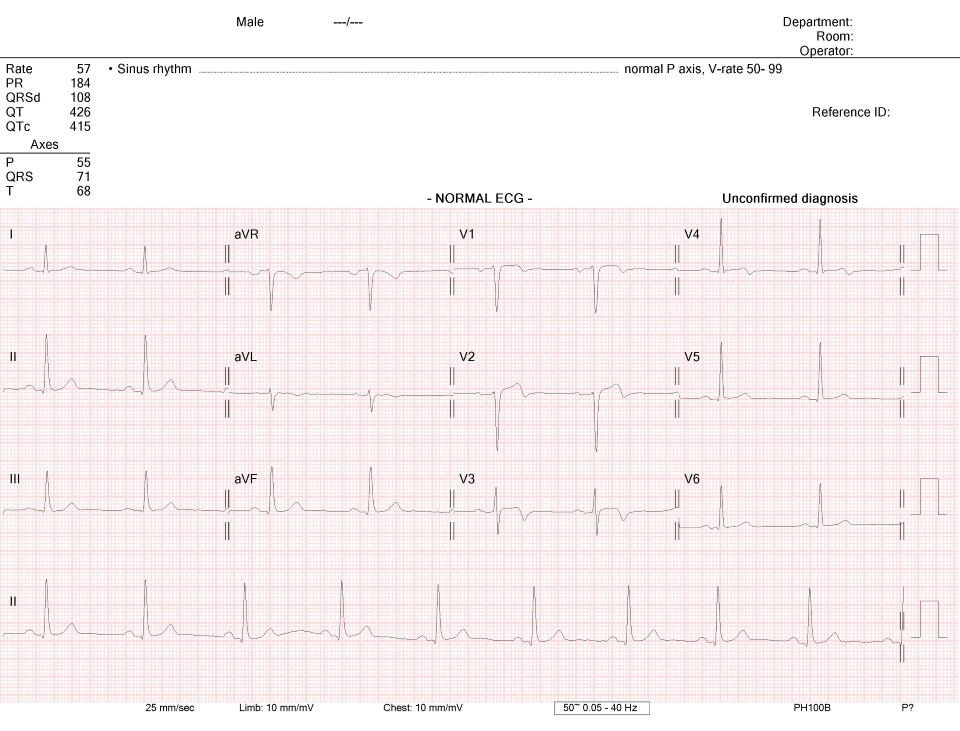
Due to the seemingly similar presentation to his previous sudden cardiac arrest, a 12 lead ECG was quickly captured.
Discussion
Whilst the patient presented as clinically well and it appeared that he had completely recovered from syncope, there are some concerning findings associated with his history and presentation. The patient had suffered a spontaneous VF arrest requiring stenting merely 6 weeks ago; his echocardiogram was normal and angiogram revealed some mild LAD stenosis.
The ECG shows a biphasic T-wave in lead V2 and deep inversion in V3; there is also T wave inversion in V1&4. This is clinically significant with Wellens’ Syndrome and should be treated as potentially life threatening. Wellens’ Syndrome is identification of critical coronary stenosis, primarily of the LAD. These patients often require invasive intervention and do poorly with medical management. They are highly likely to suffer sudden extensive anterior wall STEMI or cardiac arrest. The understanding of the T-wave pattern is that of transient acute STEMI followed by reperfusion with symptom resolution and morphing T-waves. The myocardium remains unstable however and can suddenly re-occlude at any time, with normalisation then hyperacute T-waves followed by acute STEMI or arrest. This may not necessarily be captured on a standard 3 lead ECG and is a stark reminder to everyone that the diagnostic benefits of a 12-lead ECG over what a 3-lead ECG can provide simply cannot be understated.
Treatment
Given the high potential for sudden arrest in this case, a very gently approach was undertaken. An 18ga PIVC was inserted for safe transport in case of acute deterioration and pre-hospital blood samples drawn. The patient was loaded on the stretcher without any physical exertion. Aspirin and GTN were withheld as the patient was asymptomatic and already on DAPT. Serial ECGs were captured and sent to the receiving emergency department. Discussion with the senior physician confirmed suspicious ECG for Wellens’ Syndrome and cardiology were contacted. The PCI lab was not activated at this stage, though we were advised to notify immediately if there was any change and to upgrade to Priority 1 conditions as appropriate. Defibrillation pads were placed readily behind the patient pillow as a precaution.
The patient remained stable throughout the transfer and upon arrival, we met the ED registrar who had lead the patients’ first VF arrest. It was confirmed that the ECG changes were new from his previous discharge and the patient was admitted under cardiology for urgent angiography.
Further reading
https://litfl.com/wellens-syndrome-ecg-library/
http://hqmeded-ecg.blogspot.com/search/label/Wellens%27%20syndrome
https://emcrit.org/emcrit/who-needs-acute-pci/
Disclaimer
*Patient has been de-identified and verbal consent was obtained authorising the use of ECG for educational purposes.
Page contributors:
Ben Robinson, AP18395
Ambulance Paramedic, Metropolitan Ambulance Service
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.