
Definition
Chronic Kidney Disease (CKD) is the progressive loss of renal function over a period of months or years, and develops as a complication of systemic diseases or as a complication of many renal diseases.
Key Terms
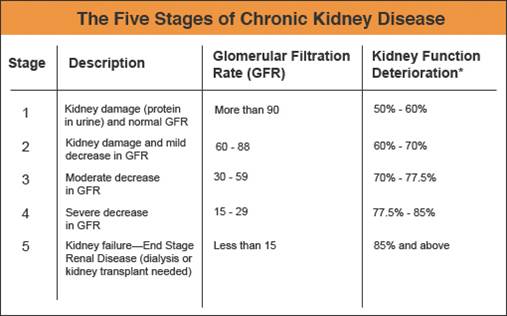
- Glomerular Filtration Rate (GFR): The metric used to estimates how much blood passes through the glomeruli each minute. Glomeruli are the tiny filters in the kidneys that filter waste from the blood. GFR is measured via the levels
of creatinine in urine.
Pathophysiology
Chronic Kidney Disease decreases the glomerular filtration rate and tubular functions with changes manifesting throughout all organ systems.
Kidneys are adaptable to loss of nephron mass and symptomatic changes as a result of increased creatinine, urea, potassium and alterations in sodium and water balance usually do not become apparent until renal function declines to less that 25% of normal functions, in which case renal compensation is depleted.
Uraemia is a syndrome of CKD and includes elevated blood urea and creatinine levels accompanied with fatigue, anorexia, nausea, vomiting, pruritis (itchy skin) and neurological changes. Uraemia represents consequences ralted to CKD including retention of toxic wastes, deficiency states and electrolyte disorders.
Risk Factors
1 in 3 Australian adults are at risk of developing Chronic Kidney Disease as result of lifestyle & biological factors such as smoking, obesity, diabetes, age > 50yrs or indigenous descent. The infographic below shows the most common risk factors.

Risk factors that are known specifically to contribute to Chronic Kidney Disease are explained below:
- Diabetes: Increased glucose damages nephron
- Hypertension: Prolonged, uncontrolled hypertension causes arterioles to harden, weaken or narrow leading to decreased blood flow to nephron = necrosis. Poor kidney function also leads to inability to control the renin-angiotensin-aldosterone system, further exacerbating hypertension.
- Poor cardiovascular health: Congestive Heart Failure impedes venous return and/or poor blood flow to kidneys
- Obesity/smoking: Increased risk of comorbidities such as hypertension and diabetes
- Aboriginal/Torres Straight Islanders are three times as likely as non-Indigenous people to have indicators of Stage 1 chronic kidney disease, and more than four times as likely to have indicators of Stages 4 and 5. The greater prevalence of chronic kidney disease in some Aboriginal and Torres Strait Islander communities is due to the high incidence of traditional risk factors, including diabetes, high blood pressure and smoking, in addition to higher levels of inadequate nutrition, alcohol abuse, streptococcal throat and skin infection, poor living conditions and low birth weight, which is linked to reduced nephron development.
Causes
There are 3 known contributing factors to Chronic Kidney Disease:
Increase glomerular pressure (GP)
As diabetes mellitus causes an increased blood pressure, the pressure coming through the afferent arteriole also increases.
Normally, the renin-angiotensin aldosterone system (RAAS) is triggered by hypotension, however an increase in glucose also triggers the RAAS which causes vasoconstriction in the efferent arteriole, thus adding to the increase in glomerular pressure. This increase in pressure in the glomerulus damages the glomeural basement membrane (GBM) and eventually allow molecules through the GBM which otherwise wouldn’t fit.
Barotrauma to mesangial cells
As mesangial cells undergo prolonged pressure, inflammation occurs which cause expansion of cells. Cell expansion damages podocytes which further stretches and damages the GBM resulting in an increased thickness to the GBM.
Nephron Ischemia
As the renin-angiotensin-aldosterone system causes vasoconstriction, the peritubular capillaries (blood vessels which wrap around the rest of the nephron) have decreased blood flow and thus decreased ability to reabsorb and secrete. This leads to loss of essential nutrients and the retention of toxins.
Initial clinical findings will include an increased glomerular filtration rate (during stage 1, however will drop as chronic kidney disease advances), increased proteinuria (especially albumin, due to mesangial expansion) and haematuria (due to nephron death).
Major causes in Australia:
Glomerulonephritis (25%)
There are a large group of diseases characterised by damage of the glomerulus. Most of the diseases are caused by inflammation in the glomeruli (increasing inflammation leads to decreasing GFR). Most commonly affected areas:
- Glomerular Basement Membrane (GBM)
- Mesangial cells
- Capillary endothelium
- Risk factors include: TB, HIV, hepatitis, cardiac defects, obesity and constant use of NSAIDs.
Hypertension (16%)
The glomerular blood pressure is approximately 60mmHg and this BP is controlled by smooth muscles (juxtaglomerular cells) surrounding the arterioles. If the systemic hypertension is uncontrolled, these juxtaglomerular cells become overworked. Eventually they weaken, harden and narrow and are unable to control BP within the glomerulus.
Hypertension within the glomerulus damages mesangial cells, podocytes and the glomerular basal membrane. Once damaged, these cells are unable to filter correctly and chronic renal failure begins.
Treatment
See Renal Dialysis
Page contributors:
 | Default Author St John WA |
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.