
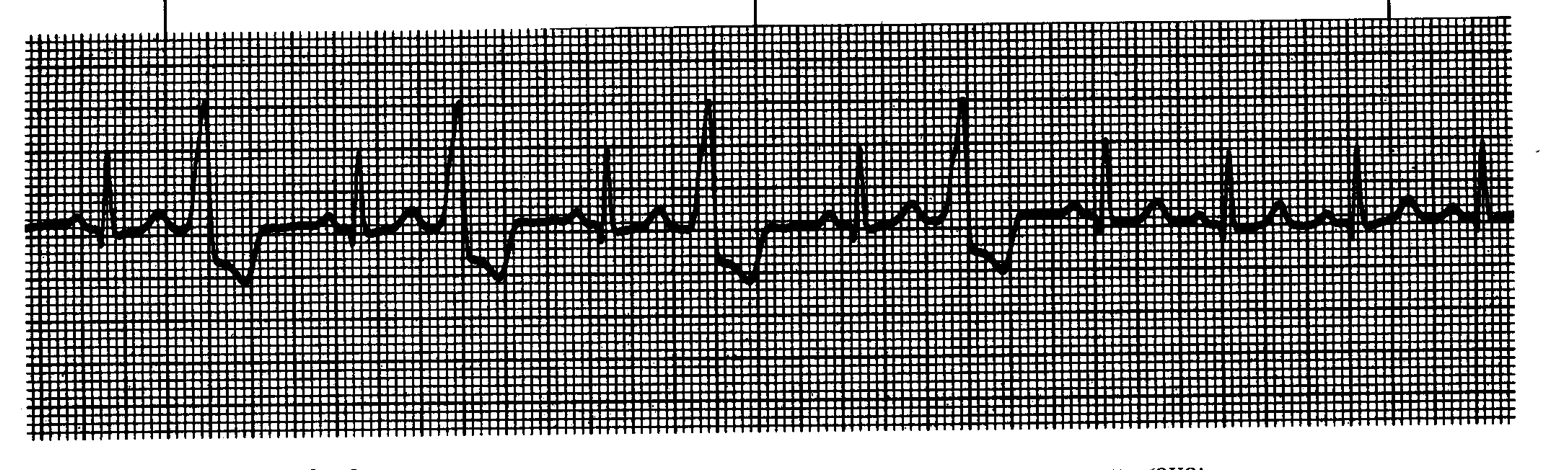
Ventricle ectopic focus premature discharge – Impulses travel using abnormal pathways resulting in an abnormal QRS complex. Bypassing the pathway causes a slow and ineffective travel as it travels cell-by-cell. The PVC can be single beat, every second (bigeminy), every third (trigemini) or run in pairs (couplets). Can occur in healthy people
| QRS Complex | P Wave | PR Interval | Rate (bpm) |
|---|---|---|---|
| >0.12s (> 3 small boxes) | Absent | Not Measurable | Varying |
- AMI
- Anxiety
- CCF
- Drug toxicity
- Excessive caffeine or alcohol consumption
- Heart disease
- Mechanical stimulation
- Reperfusion
- Chest pains
- Fatigue
- Syncope
- Hyperventilation
- Skipped beat
When the pacemaker site in the ventricles takes over as pacemaker when the AV node fails to fire at 40-60bpm. The ventricular cells fire at 20-40bpm acting as a backup generator when the AV node fails to fire. The impulses are wise and absent P-wave as there is no atria involvement.
| QRS Complex | P Wave | PR Interval | Rate (bpm) |
|---|---|---|---|
| >0.12s (> 3 small boxes) | Absent | Not Measurable | 20 – 40bpm |
- AMI or ischemia
- Pacemaker failure (AV or SA node)
- Reperfusion
- Chest pains
- Shortness of breath
- AMI symptoms
- Peripheral oedema
- Cyanosis
When inherent pacemaker site beats faster than normal rate due to enhance automaticity of ventricular tissue. Excited version of IVR but does not tolerated for long periods of time.
| QRS Complex | P Wave | PR Interval | Rate (bpm) |
|---|---|---|---|
| >0.12s (> 3 small boxes) | Absent | Not Measurable | 40 – 100 bpm |
- AMI or ischemia
- Pacemaker failure (AV or SA node)
- Reperfusion
- Chest pains
- Shortness of breath
- AMI symptoms
- Peripheral oedema
- Cyanosis
- Palpations
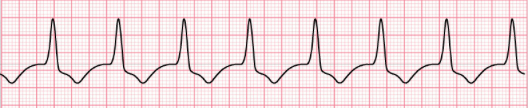
When dominant ectopic site in ventricles take control of heart pacing. VT may self-terminate or sustained. Causes difficulty to fill the heart between contractions to maintain cardiac output.
Self-terminating VTs may show minimum three (3) consecutive PVC’s.
| QRS Complex | P Wave | PR Interval | Rate (bpm) |
|---|---|---|---|
| >0.14s (> 3.5 small boxes) | Absent | Not Measurable | 140 – 250 bpm |
- AMI or ischemia
- Cardiomyopathy
- CCF
- Drug toxicity
- Electrolyte disturbance
- Heart disease
- Medications that prolong QT interval
- Reperfusion
- Light-headedness
- Palpations
- Fatigue
- Chest Pains
- Syncope
- Shortness of Breath
Polymorphic VT where QRS complex changes from negative to positive amplitude – Associated with prolonged QT interval causing wide QRS.
| QRS Complex | P Wave | PR Interval | Rate (bpm) |
|---|---|---|---|
| >0.14s (> 3.5 small boxes) | Absent | Not Measurable | 140 – 250 bpm |
- AMI or ischemia
- Cardiomyopathy
- CCF
- Drug toxicity
- Electrolyte disturbance
- Heart disease
- Medications that prolong QT interval
- Reperfusion
- Light-headedness
- Palpations
- Fatigue
- Chest Pains
- Syncope
- Shortness of Breath
Coarse VF:
Fine VF:
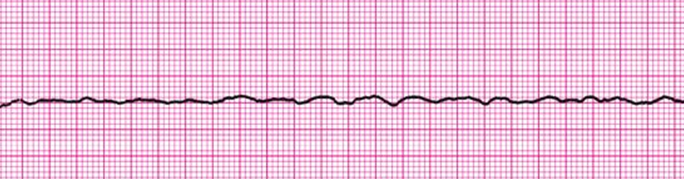
Lethal arrythmia resulting in chaotic electrical discharges from multiple foci in the ventricles. There is no cardiac output as it cannot beat in an organised fashion.
| QRS Complex | P Wave | PR Interval | Rate (bpm) |
|---|---|---|---|
| None | Absent (Coarse or fine wave) | Not Measurable | None |
- AMI
- Electrolyte disturbances
- Preceded by other arrythmias
- Cardiac Arrest causes (4 H’s & 4 T’s)
- No signs of life
- Absent or abnormal breathing
- Loss of consciousness
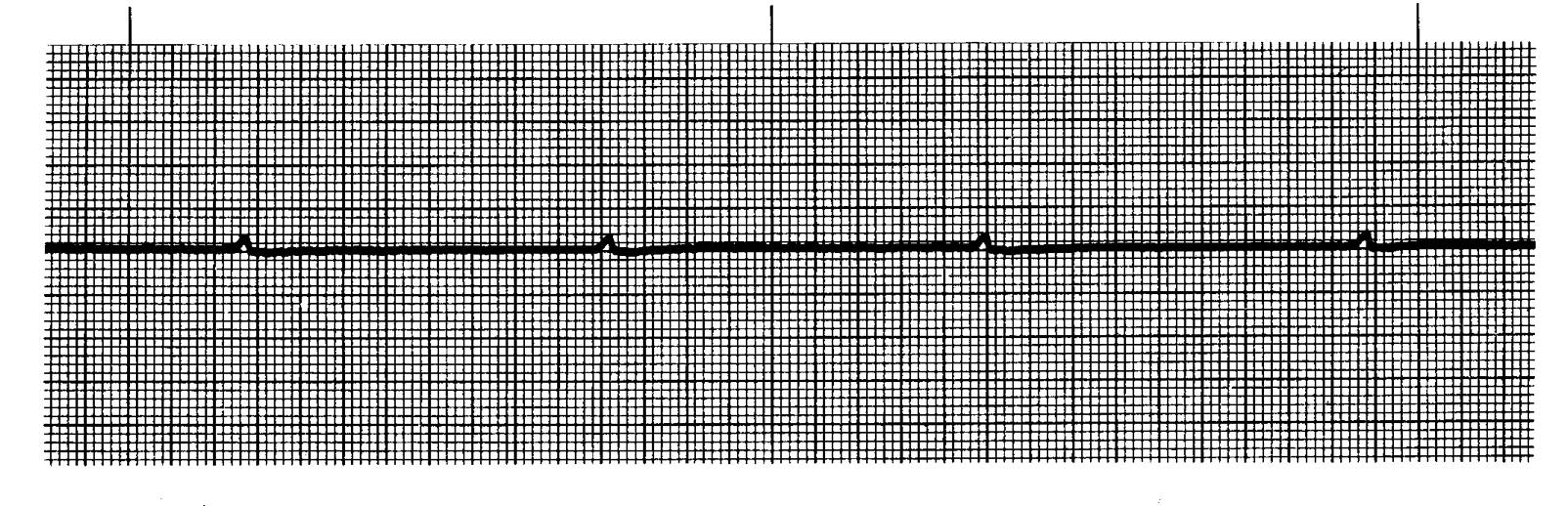
Series of P-wave which slows ventricular standstill (no ventricular activity); this usually generates into asystole. Treat as if asystole.
| QRS Complex | P Wave | PR Interval | Rate (bpm) |
|---|---|---|---|
| None | May be present but not sustainable | Not Measurable | None |
- AMI
- Electrolyte disturbances
- Preceded by other arrythmias
- Cardiac Arrest causes (4 H’s & 4 T’s)
- No signs of life
- Absent or abnormal breathing
- Loss of consciousness
Page contributors:
 | Thanh Bui, AP60825 Event Medic, Emergency Medical Technician & Volunteer Development Officer
|
 | Andrew Moffat, AP16790 |
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.