
Management of the controller and its alarm functions will be predominately undertaken by the patient or their carer who has been trained in use of the VAD and its maintenance. Paramedics should not attempt to troubleshoot the VAD device without the assistance of the patient/carer or the advice of the FSH staff unless the patient is clearly critical. It is important to recognise that not all VAD patients will have a carer with them at all times.
The patient should be treated symptomatically as per Clinical Practice Guidelines.
- Emergency Alarm: Red light illuminated on controller + loud continuous alarm tone
- Potential causes:
- No battery or power sources
- Driveline damaged/disconnected
- Controller malfunction
- Assess patient
- The patient, carer or emergency care provider should;
- Confirm pump has actually stopped (auscultation, ‘Pump stopped’ alarms)
- Check all pump & power connections to controller are intact and re-establish if not
- Swap to spare controller – as per instructions kept with patients equipment. Contact FSH for instruction
- Follow resuscitation guidelines
Perform resuscitation as per normal guidelines taking note of the following:
CPR
- There may be risks associated with performing external chest compressions due to potential disruption of the outflow graft. However, if the pump has stopped and the patient is severely compromised chest compressions will keep some blood pumping out of the native heart valves. Contact the AHFCTS team at FSH immediately.
- Do not disconnect the driveline during CPR.
Defibrillation
- Anterior-Posterior (AP) defibrillator pad placement required (avoid apex pad placement as this is right over the VAD pump and could interrupt function)
- Put controller and batteries on the bed/trolley with the patient and treat as part of them during defibrillation (paramedic/carer not to hold the equipment. Do not use mains power as a power source during defibrillation).
- Patient may be haemodynamically stable in a normally life threatening arrhythmia. There may be time to contact the AHFCTS team
- Never disconnect the driveline from the controller or the batteries for defibrillation
- If the pump has stopped you will be unable to hear it’s whirring on auscultation over the chest (left side for LVAD, right side for RVAD) - patient may or may not be compromised depending on the extent of underlying cardiac damage/recovery.
- Thrombus formation is likely in prolonged pump stop situation – restarting the pump if it has been stopped for > 5mins can be dangerous
Note: Ambulance staff are encouraged to contact the Advanced Heart Failure and Cardiac Transplant Service at Fiona Stanley Hospital at any time for advice regarding the patient’s usual health state and advice regarding complication/issue management. Please call (08) 6152 2222 and ask for the Cardiac Transplant Consultant on-call.
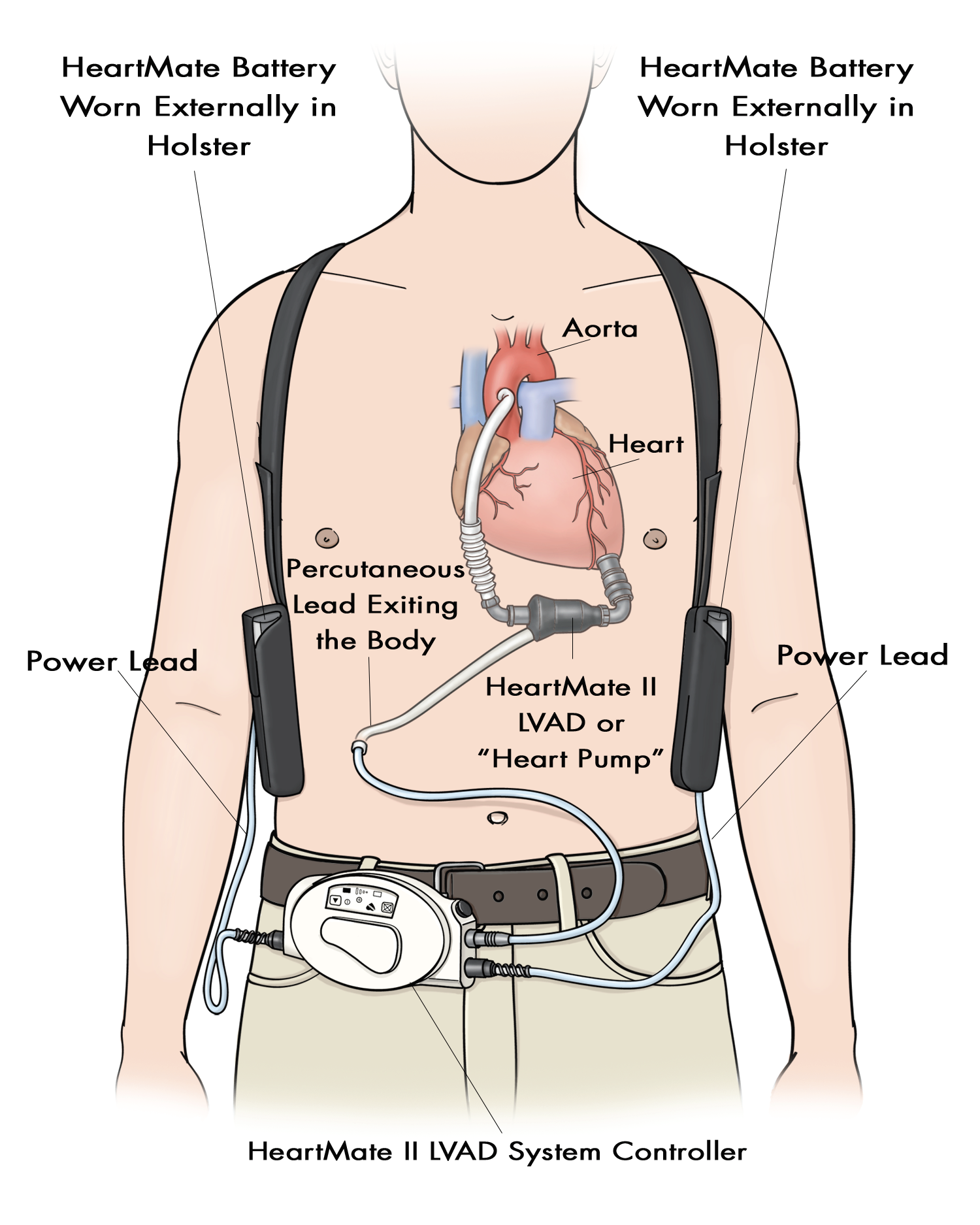
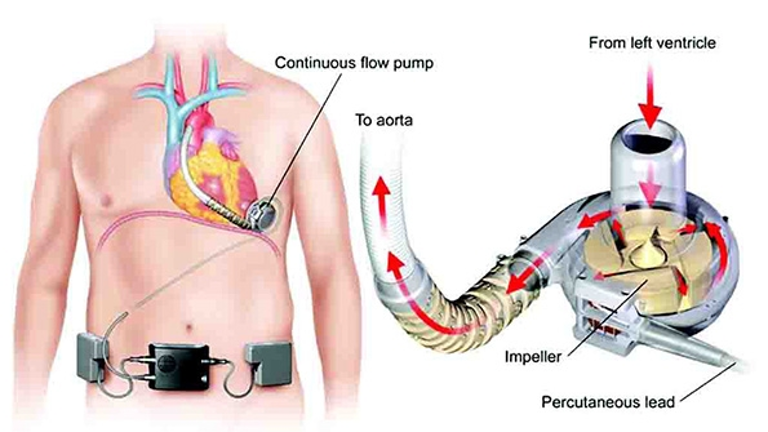
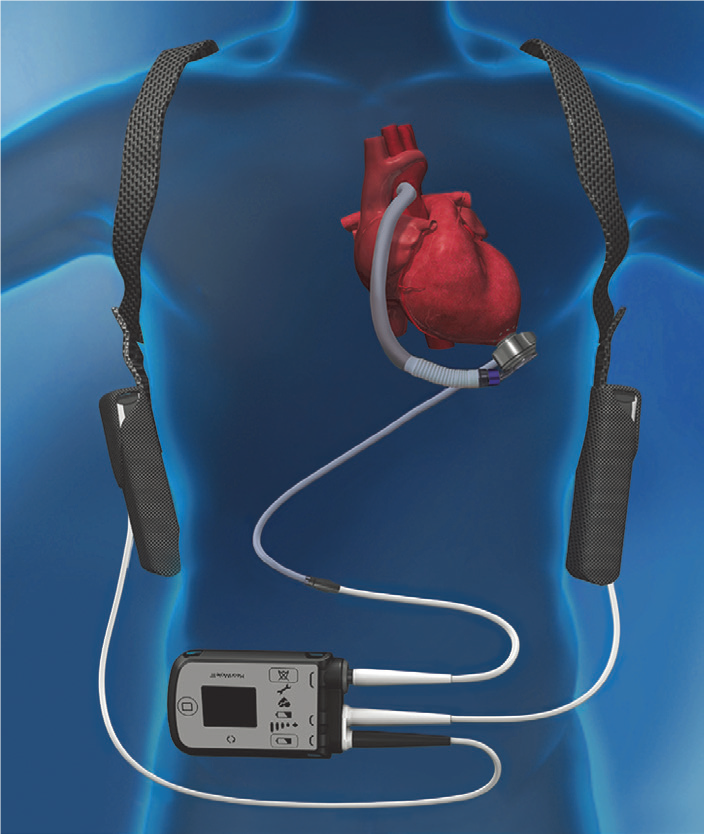
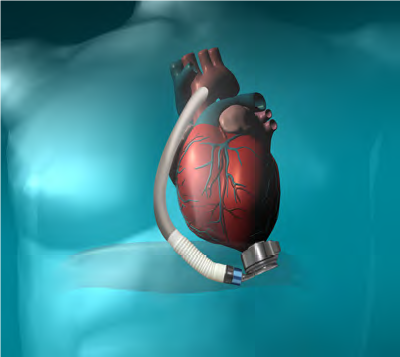
A Left Ventricular Assist Device, commonly known as an LVAD or VAD, is a mechanical circulatory assistance device that is used to partially or completely replace the function of a failing left ventricle. These LVADs are generally intended for longer term use (months to years and in some cases for life) and are mostly for patients suffering from congestive heart failure.
VADs are used to help patients have an improved quality of life with decreased heart failure symptoms. VADs are used as a:
- Bridge To Transplant – keep patient alive until a suitable donor heart is available
- Destination Therapy – patient not suitable for heart transplantation but deemed appropriate for a VAD.
- Bridge to Recovery – Occasionally, but not often, a patient’s heart function can improve with the VAD so it can later be removed without the patient requiring a transplant
VADs are usually designed to assist the left ventricle (LVAD), but occasionally can be inserted on the right side (RVAD), or both ventricles at the same time (BiVAD). The configuration used can depend on factors including the underlying heart disease, right and left ventricular function and the pulmonary arterial resistance.
With medical and device advances, VADs have improved significantly in terms of providing improved survival and quality of life among recipients. Ventricular Assist Device therapy patients are only managed in Western Australia by the Advanced Heart Failure and Cardiac Transplant Service at Fiona Stanley Hospital. There are currently 15-20 patients in the community on VAD support.
There are three main types of longer term VADs used in Western Australia – the Heartmate 3®, the HeartWare HVAD® and the Thoratec HeartMate II® VAD. The components, function, routine monitoring and complication profile are similar between devices.
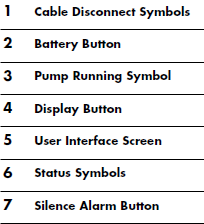
Types of VADs in use at Fiona Stanley Hospital
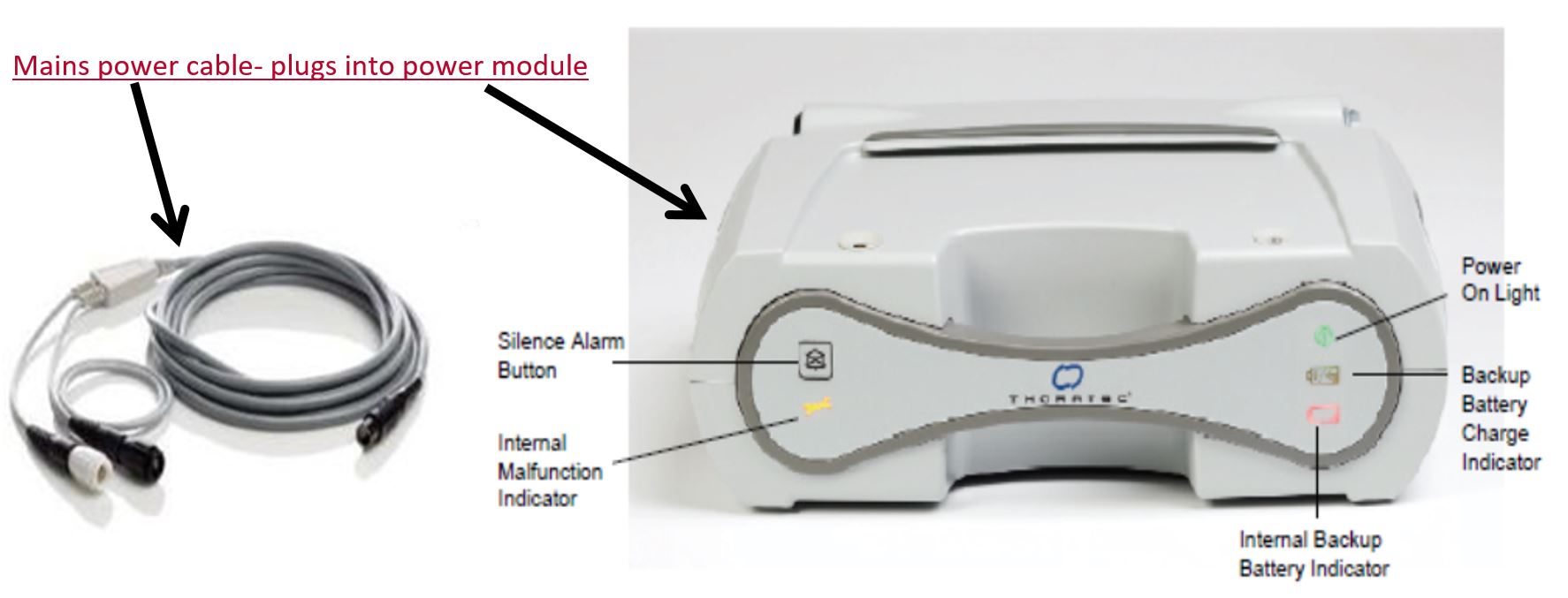





Mobile Power Unit
All VADs consist of the following components:
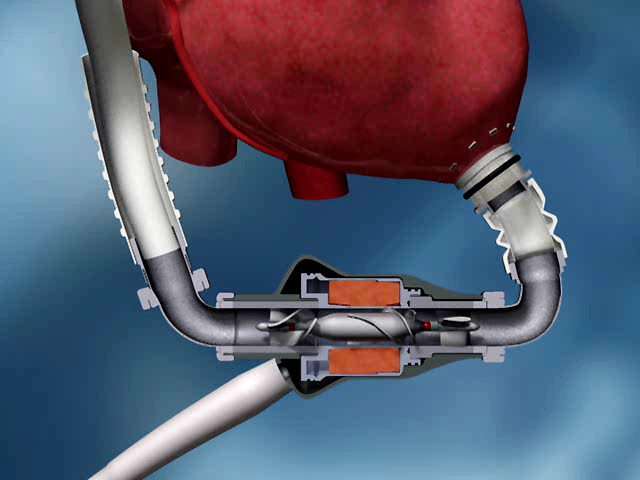
Blood pump
- Pump with a single moving part – the rotor propels blood forward
- Rotor supported by hydrodynamic or magnetic forces, or by bearings
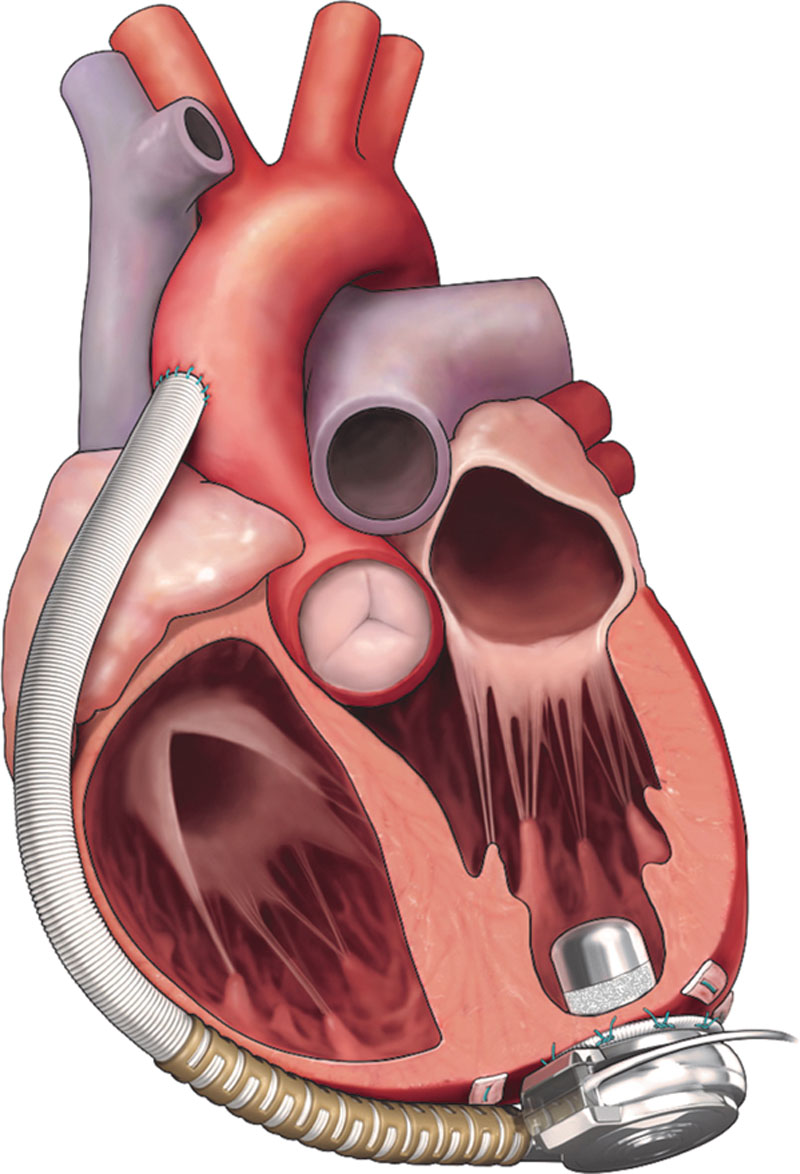
Inflow and Outflow Cannulae
- Blood is delivered to the pump via an inflow cannula that is inserted into the ventricle in which it is supporting (left ventricle for an LVAD, right atrium/ventricle for an RVAD)
- Blood is returned to the body from the pump via an outflow cannula that is anastomosed to an artery (ascending aorta for an LVAD, pulmonary artery for an RVAD)
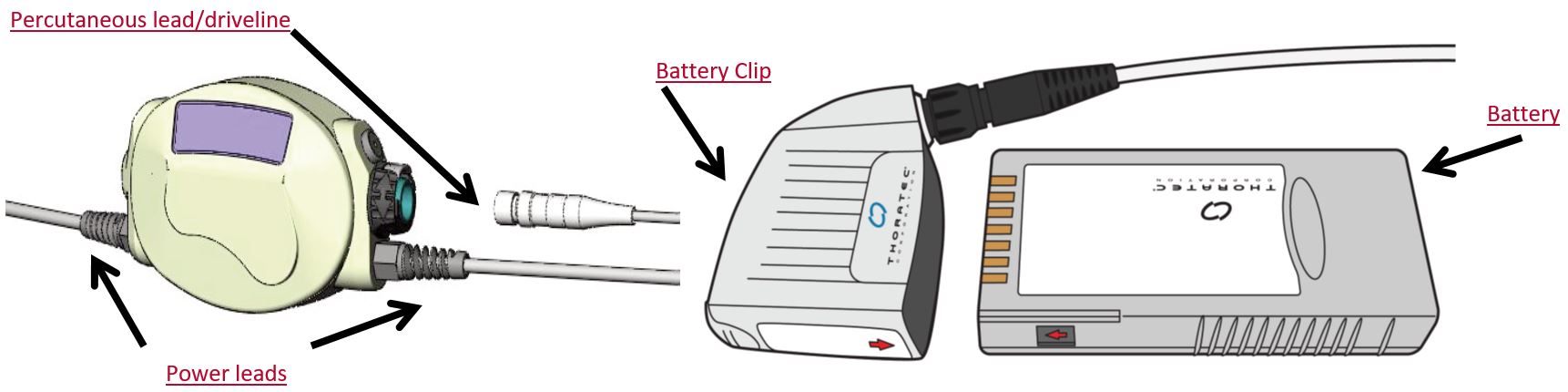
Percutaneous Lead (Driveline)
- Contains wires connecting the pump inside the patient to an external controller and power
- Tunnelled subcutaneously. Exits the body from the abdomen
- Caution needs to be used to ensure the lead is not damaged
- Caution with liquids coming into contact with driveline
- Driveline exit site on abdomen to be kept immobile & patient/carer attend to dressing with aseptic technique – prevents infection
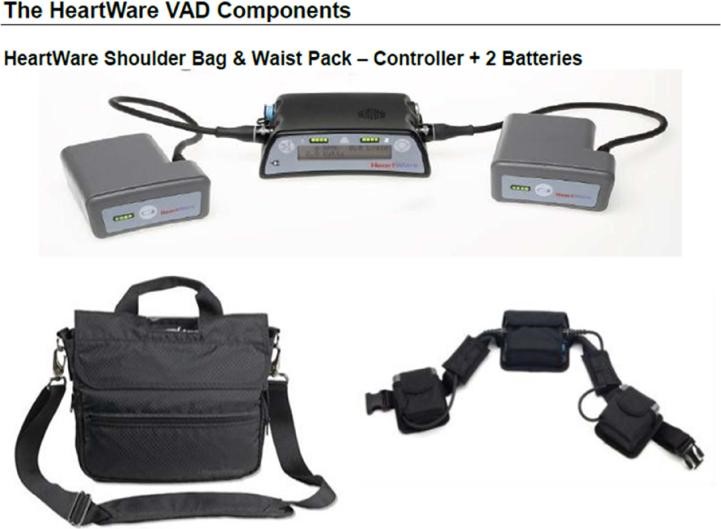
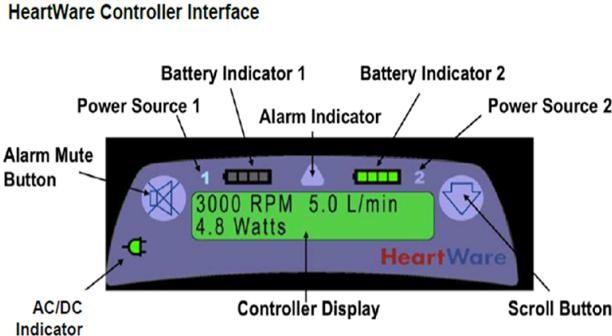
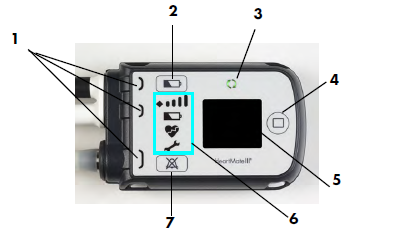
Controller
- Driveline connects into the controller
- This is a computer which tells the VAD pump how to operate
- The HeartMate II® controller does not display any parameters
- The HeartWare HVAD® and the Heartmate 3® controller displays operating details to the patient/clinician
- Blood flow estimation in L/min
- Speed in RPM
- Power in Watts
- Both device controllers give sound/light if alarm condition occurs (HeartWare HVAD® and Heartmate 3® screen message)
Power Sources
- 2 power sources need to be connected at all times
- Configuration depends on the type of VAD however essentially:
- 1. 2x batteries (used during the day as allows patient to be portable)
- Battery to be changed when low to ensure 2 reliable power sources at all times
- HeartWare® device depletes one battery at a time, HeartMate II® and Heartmate 3® depletes both batteries together
- 2. Mains/AC Power (used overnight to allow uninterrupted sleep).
- For the HeartWare® device one battery is also always connected in case of power failure/blackout.
- For the HeartMate II® device there is an emergency battery up supply (max 30mins) in the back of the AC Power Base Unit (PBU) if they are connected to mains power.
- For the Heartmate 3® device, there is an emergency backup battery in the controller that will last approximately 15 minutes if both power leads are disconnected from the AC power/batteries.
- 1. 2x batteries (used during the day as allows patient to be portable)
- If BOTH power sources are disconnected from the controller, the VAD will stop (except for the Heartmate 3®, see above)
- This causes continuous alarm tone & no lights/message on the controller screen
- Reconnect power immediately
Patient Assessment

VADs continuously unload the ventricle throughout the cardiac cycle. They are referred to as ‘continuous flow’ devices. Often the aortic valve does not open (or not open fully) as most of the blood flow is exiting the heart via the VAD. Due to this, the patient often will not have a palpable pulse. If a pulse is not palpable a standard blood pressure measurement will not be possible. In the hospital setting blood pressure is obtained using a Doppler device.
Other techniques can be used to assess a patient’s cardiac output state. These include assessing for warmth, colour, capillary refill, mentation and checking for LVAD parameters or alarms. If the LVAD is running, a mechanical whirring sound should be heard over the heart.
The patient &/or carer/relative may be able to give an account of the patient’s usual condition.
There often remains a degree of pulsatility so it is therefore beneficial to still attempt pulse oximetry monitoring but this may be inaccurate (falsely low or unrecordable).
LVAD patients still have their own active heart rhythm so can be monitored and have ECGs. They are still susceptible to arrhythmia as the unsupported right ventricle still needs to send blood efficiently to the left ventricle.
VAD patients may often have an Automated Implantable Cardioverter Defibrillation device. VT may be well tolerated especially in patients with combined LVAD and RVAD support. If the patient is in VT but looks and feels well, there is often time to contact the AHFCTS team for advice. Don’t forget the patient and their carer are experienced in managing their LVAD and are a great source of information/advice in VAD assessment.
Potential Complications
Possible complications for a patient on a VAD include:
Infection
- Due to having a foreign body implanted in their body
- Typical sites for infection include the VAD exit site (driveline site) or blood stream
Bleeding
- Due to LVAD dynamics and anticoagulation/antiplatelet medications (most are on Aspirin and Warfarin)
- GI bleeding is not uncommon with continuous flow VADs. Epistaxis also can occur
Stroke
- Can be due to a clot moving from the heart/pump to the brain
- Can be a haemorrhagic stroke due to anticoagulation
Arrhythmias
- Occur as commonly as other patients but may be better tolerated.
- Can be due to VAD inflow cannula irritating the heart muscle
Low flow/Suction alarms
- Decreased venous return getting back to heart and into pump
- Dehydration
- Bleeding
- High blood pressure
Device malfunction
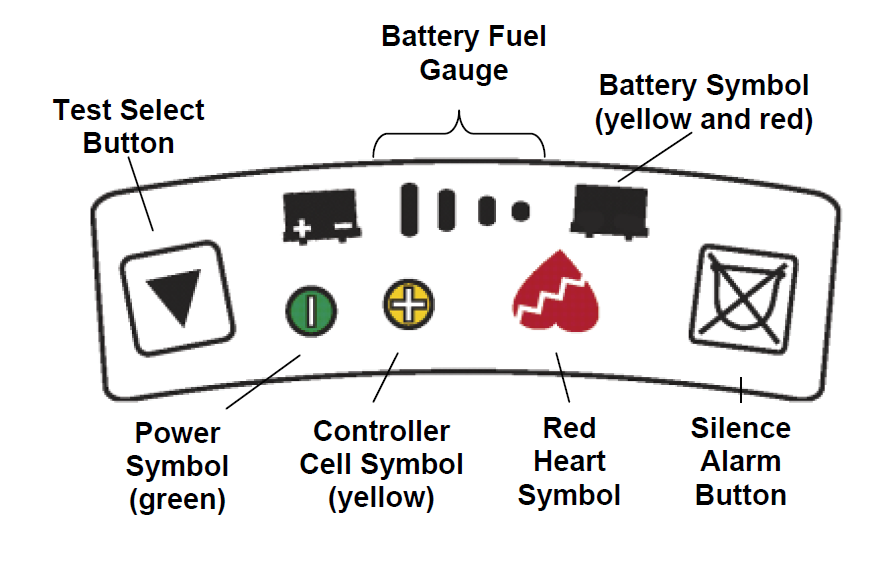
CAUTION: Never disconnect power from both controller leads at the same time.
- Prepare for power change (See your Patient Handbook)
- Remove only one battery or the white PBU cable from the controller
The power symbol will flash and the alarm will sound once every 4 seconds. - Connect the new fully charged battery or white PBU cable to the controller
- Wait until the power symbol stops flashing and the alarm stops
- Remove the second battery or cable from the controller.
The power symbol will flash and the alarm will sound - Connect the fully charged battery or black PBU cable to the controller.
- Wait until the power symbol stops flashing and the alarm stops
- Check fuel gauge
- The pump will stop if power is removed from both controller cables at the same time.
- If power to the controller is interrupted, firmly press the Test Select button (up arrow) or the Alarm Reset Switch to restart the pump.

CAUTION: Never disconnect power sources from the controller at the same time.
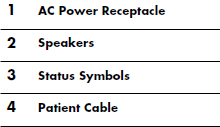
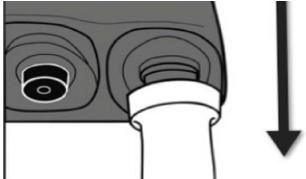
- Disconnect the Battery with the least remaining charge by rotating the connector in the direction of the arrow.
- Grasp the cable of the new Battery or the AC Adapter near the connector, leaving the connector free to rotate.
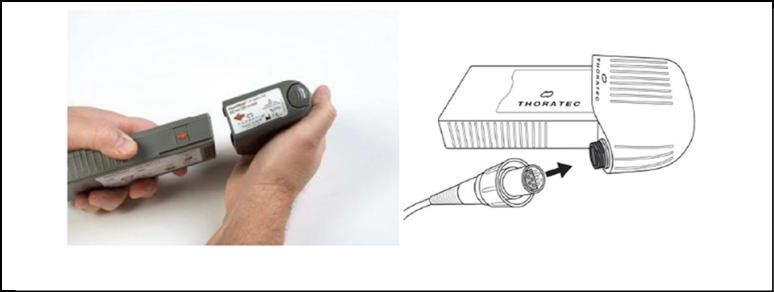
- Line up the solid white arrow on the connector with the white dot on the Controller
- Push the cable firmly onto the Controller until it locks in place.
- When pushing the connector onto the Controller the white arrow will shift slightly.
- Correct locking position: White arrow aligned with white dot on Controller.
- The pump will stop if power is removed from both controller cables at the same time.
- Sit or lie the patient down.
- Ensure the replacement Controller within reach, along with batteries/ clips or PBU cable.
- Rotate the perc lock on the replacement Controller in the direction of the “unlocked” icon until the perc lock clicks into the fully-unlocked position
- Repeat Step 3 for the patients Controller until the perc lock is in the fully-unlocked position.
- Attach the power leads on the new, replacement Controller to the PBU cable or to the battery clips, depending on the power source being used.
- If using battery power, place fully-charged batteries into the clips after attaching the power leads.
- Press the Silence Alarm Button for 3 seconds on the replacement Controller to silence its Red Heart Alarm for two minutes.
- Disconnect the perc lead from the original Controller by pressing the metal release tab on the connector socket. The pump will stop and a continuous alarm will sound. Note: The alarm will continue until power is removed from the original Controller.
Getting the replacement Controller connected and the pump restarted is the first priority.

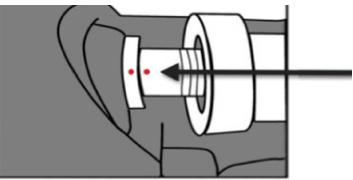
- Connect the perc lead to the replacement Controller:
- Line up the mark on the perc lead connector with the mark on the metal tab of the new Controller.
- Fully insert the connector into the socket of the new Controller (Figure 30). The pump should restart/alarms should stop. Note: Gently tug on metal end of the lead to assure that it is fully engaged into the socket. Do NOT pull on the lead.
- The pump should restart, skip to Step 12 OR If the pump does not restart and the RED HEART ALARM continues:
- Firmly press the Silence Alarm or Test Select button to restart the pump.*
- Check the power source. Ensure that power is going to the Controller.
- Assure the perc lead is fully inserted into the socket. Gently tug on the metal end. Do NOT pull the lead.
- If the pump still does not restart, attempt to restore pump function using the System Controller backup system:
- Simultaneously press and hold the Test Select and Silence Alarm buttons.
- The Red Heart Alarm will stop and an Advisory Alarm will occur with a repeating cycle of one beep per second for two seconds, followed by two seconds of silence to indicate that the System Controller is operating on the backup system.
- After the pump restarts, rotate the perc lock on the new, replacement Controller in the direction of the “locked” icon until the perc lock clicks into the fully-locked position.
- Disconnect power from the old, original Controller. The original Controller will stop alarming once power is removed.
- Sit or lie the patient down.
- Place the new Controller within easy reach.
- On the patients Controller slide the white static protection sleeve up the driveline away from the controller to exposed the silver driveline connection.
- Connect the new Controller to two power sources (Batteries, AC Adapter). An alarm will sound until both power sources are connected.
- To connect power sources: Line up the solid white arrow on the connector with the white dot on the Controller see page 9.
- Disconnect the Driveline from the patients Controller by pulling the two metal connectors apart.
- Connect the Driveline to the new Controller (align the two red marks and push together).
- Push the cable firmly onto the Controller until it locks in place.
- The pump should restart after a few seconds and the alarm should stop.
- If the pump does not restart, call for medical assistance immediately.
- Insert the Alarm Adapter into the Blue Connector on the patients original Controller.

- Disconnect the original Controller from power sources (Batteries, AC Adapter or DC Adapter) by gently turning the connector counter-clockwise and then gently pulling. The alarms should resolve.
Liaise with the Advanced Heart Failure & Cardiac Transplant Service at Fiona Stanley Hospital Regarding Treatment
Specialists at Fiona Stanley Hospital are available 24 hours per day and should be consulted with regarding your assessment findings and recommended treatment. The phone numbers are carried by the patient at all times and can be found on their back up equipment carry bag. The patient is to be transported to FSH wherever possible as staff there have training in this device and monitoring equipment is available
If a VAD patient is to be taken to Fiona Stanley Hospital all of their VAD equipment is to be brought with them (including spare controller, spare batteries, mains/AC power unit, battery charger)
Contact Details for Fiona Stanley Hospital VAD Team Members
- Monday – Friday 0800-1600hrs
- (08) 6152 5783
- Heart Failure/Transplant Consultant On-Call:
- via Fiona Stanley Hospital Switchboard (08) 6152 2222
Acknowledgement
Adapted from “Left Ventricular Assist Devices- Ambulance Management” Version 4-July 2015. Courtesy of the Alfred Hospital.- This information has been collated using resources from the Alfred Hospital. Pictures obtained from HeartWare and Thoratec websites, presentations and documentation. Information has been reviewed and adapted for use at Fiona Stanley Hospital by Dr Jay Baumwol (Heart Failure Consultant), Helen Hayes (VAD Nurse Practitioner) and Julie Barber (Clinical Nurse Consultant) Oct 2020.
References
- Slaughter, M. S. et al (2010): Clinical Management of Continuous-flow Left Ventricular Assist Devices in Advanced Heart Failure, Journal of Heart and Lung Transplantation. 29(4S)
- Dr. Angeline Leet presentation, Heart Failure Consultant, Alfred Hospital Shah, K. B. et al (2010): Implantable mechanical circulatory support: demystifying patients with ventricular assist devices and artificial hearts.
- Clinical Cardiology. 34(3):147-152 Fitzpatrick, J. R. (2010): Mechanical Circulatory Assistance-an evolving therapy. Circulation Journal. Dec 2010 online
Page contributors:
 | Default Author St John WA |
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.