
Important for circulation (pulmonary & systematic) of fluids, nutrients and blood around the body to keep tissues alive. Heart’s action can change based on the situation change impacting circulation, volume and pressure.
The heart is one-way valved that operates systematically:
- Fist size
- Located more towards left side of chest
- Responds to homeostatic changes
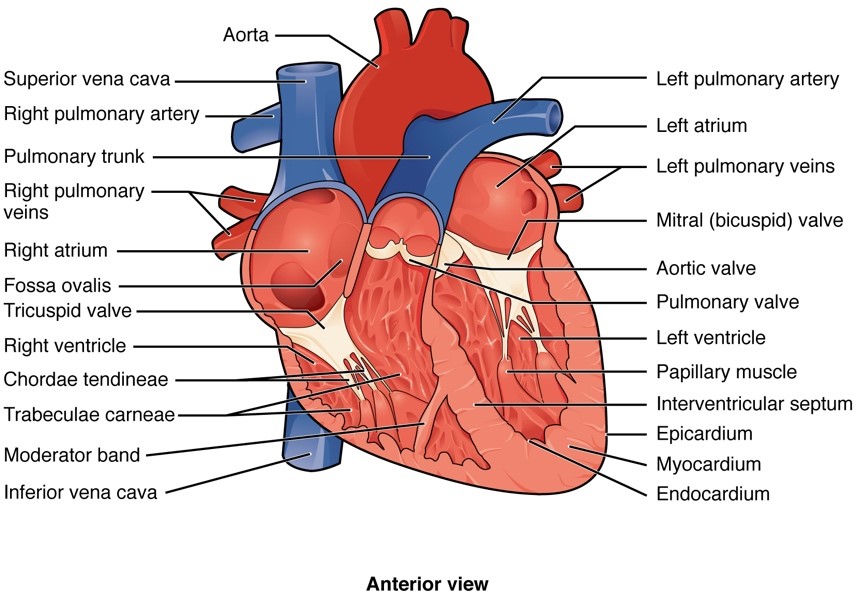
- Right Atrium (from body)
- Left Atrium (from lungs)
- Right Ventricle (from right atrium – move blood to pulmonary trunk [artery])
- Left Ventricle (from left atrium – move blood to aortic arch then to body)
Contains Trabeculae (Ventricles) & Pectinate (Atria) ridges which allow continuous bloodflow without clots
- Vena Cava Deoxygenated blood to Right Atrium
- Pulmonary Vein Oxygenated blood to Left Atrium
- Pulmonary Trunk Deoxygenated blood to Lungs for gas exchange from right ventricle
- Aorta Oxygenated blood from left ventricle
Atrioventricular Valves (AV)
- Tricuspid Between right atrium & ventricle
- Bicuspid Between left atrium & ventricle
Semilunar Valve (SL)
- Right SL Valve (Pulmonary) Right atrium & ventricle junction
- Left SL Valve (Aortic) Left atrium & ventricle junction
Vary from person-to-person, heart has a large muscle mass and needs bloodflow to deliver oxygen and remove CO2
- Blood supply comes from aortic root (the ostia)
- Artery travel on heart surface (sulci)
- Smaller branches penetrate myocardium
- Ostia has two (2) artery openings; Right & Left Coronary Artery
- Cardiac veins return to coronary sinus (posterior heart)
- Deoxygenated blood from coronary sinus empty into right atrium
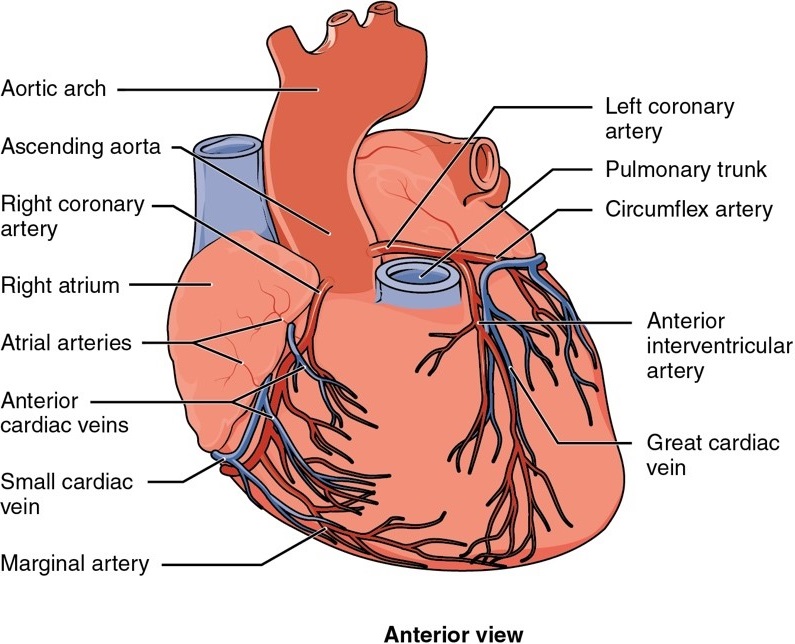
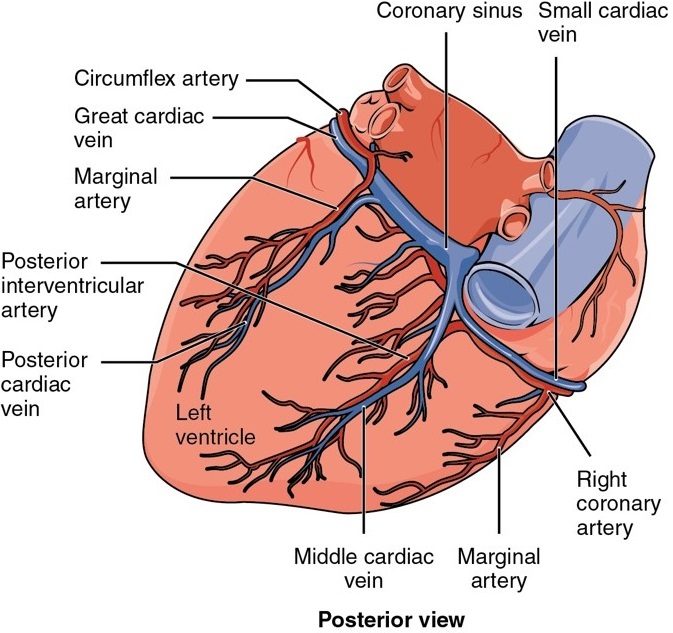
Right Coronary Artery (RAD): Inferior Region
- Supplies to inferior section of the heart – inferior wall of left & right ventricles and SA & AV nodes.
- Branches half-way along right ventricle then split distally into posterior descending & posterolateral artery
Left Main Artery (LM / LCA): Anterior Region
- Branches into left anterior descending (LAD) and circumflex (Cx) artery – Supplies to anterior wall of left ventricle and anterior portion of interventricular septum and bundle branches
- LAD is diagonal branch
- Cx branch is obtuse marginal and supplies
Circumflex (Cx): Lateral Region
- Branched off the LCA with arteries supplying to lateral and posterior walls of the left ventricles
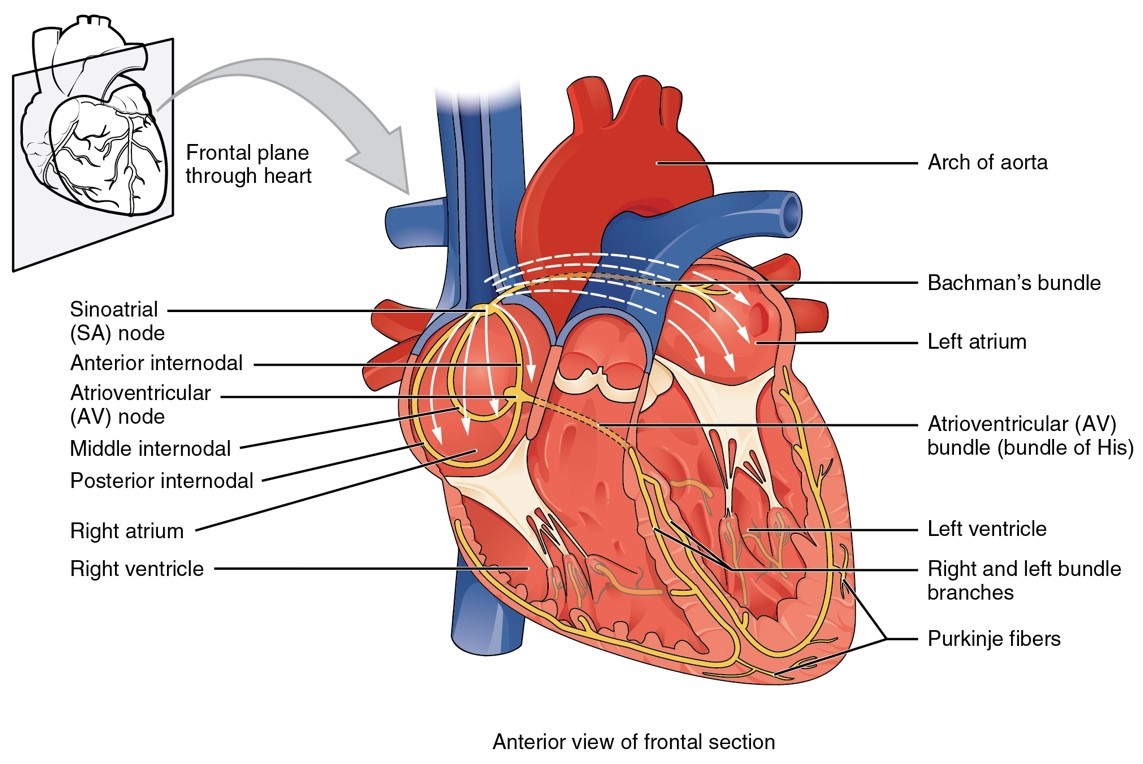
Sinoatrial Nodes (SA Node): 60-100bpm
Oval-shaped near superior vena cava – Generates automatic depolarisation impulses modified by the Autonomic Nervous System (ANS). Primary pacemaker has the most intrinsic rate of depolarisation
The impulse is sent to atria through the internodal pathways where atrial will send impulse to AV node.
Atrioventricular Nodes (AV Node): 40-60bpm
Serves as a bridge between atria & ventricles (located in atrial septum) – receives impulse and delays It before conducting the ventricles; this delay is so the atria can fill up adequately before ventricular contraction.
Additional structures (to the SA node) that can serve as pacemakers – Term ‘latent’ refer to its role when the SA node fails. These nodes can assume the role of pacemaker as (normal autonomy) to prevent cardiac arrest
- Atrial myocardium (primary): Atrial myocardial cluster cells at the coronary sinus and inferior vena cava that serve as contractile cells (not conduction cells)
- Myocardium surrounding the AV Node (secondary): Cell clusters around the AV node that can be autonomic
- His-Purkinje Network (tertiary latent): Bundle of His & entire Purkinje network can possess automaticity if all other latent pacemakers fail.
Bundle of His (AV Bundle): 40-60bpm
From AV node impulse – Splits impulse into left & right bundle branches – Subsequently branching into smaller bundles into Purkinje fibres.
Purkinje Fibres (PKF): 20-40bpm
From AV Bundle – Fast impulse (4m/sec) which runs through endocardium where impulse is sent to myocardial contractile cells (some extend into myocardium). Ventricular contraction therefore begins in endocardium and spread to epicardium
Cardiac Cycle:
- SA node activity begins, atrial activation begins (t = 0ms)
- Stimulus spreads across atrial surface, impulse reaches AV node (t = 50ms)
- AV node delays impulse from spreading by ~100ms as atrial contraction begins (t = 150ms)
- Impulse reaches AV bundle & PKF then papillary muscle (t = 175ms)
- PKF distribute impulse to ventricles (atrial contraction completed); then ventricle contracts (t = 225ms)
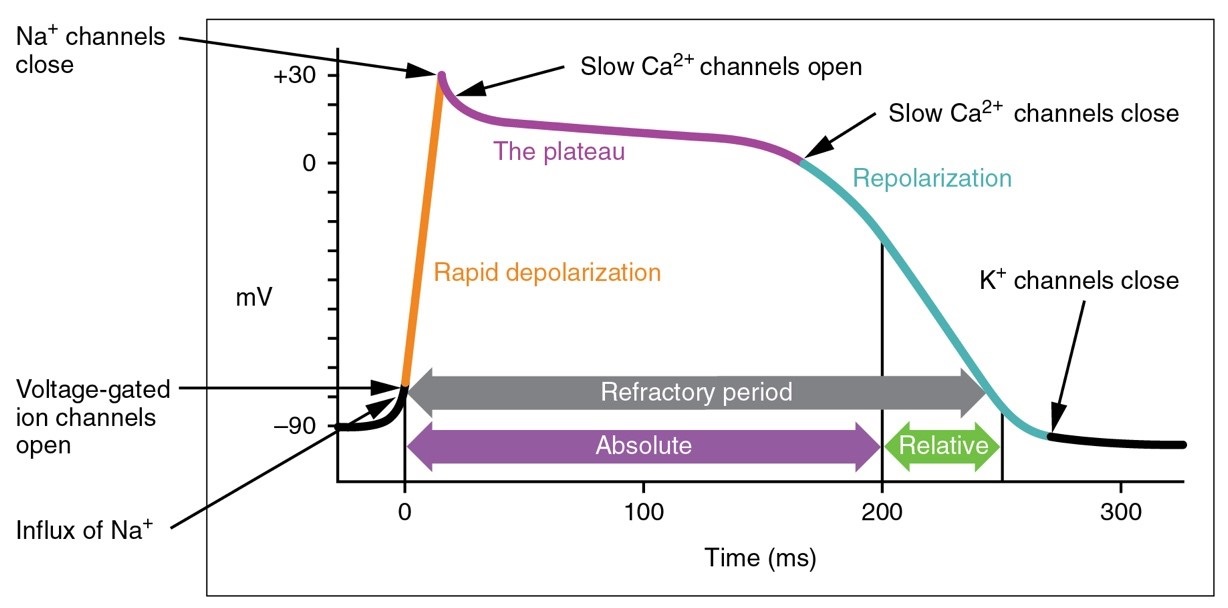
Cardiac Electrophysiology:
Cardiac cycle begins at cell-level where particle movement between cell membrane creates action potential which is transmitted along the conduction pathway – Done in five (5) stages. Any changes in electrolyte values (Na+ / Ca+ / K+) can affect cell’s action potential.
- Resting Membrane Potential (Phase 4): -85 to -95mV Heart chamber diastole
- Resting, isoelectric awaiting external stimulus (ie. Adjacent cell) or spontaneous depolarisation without influences (cardiac muscle automaticity). Resting mV is determined by membrane permeability to ions. Outside more charged than inside (more Na+ & K+)
- Depolarisation (Phase 0): Charged to +30mV (~65mV) Ventricular myocardium depolarisation
- Comes from SA node creating sudden voltage change on cell surface resulting rapid Na+ influx into cell as sodium channel opens shifting resting mV. Ca+ ions enter cell at the threshold voltage (~65mV).
- Early Rapid Repolarisation (Phase 1): +20 to 0mV
- The sodium channel closes, and brief partial repolarisation occurs as result of K+ moving outwards reducing the cell voltage.
- Plateau (Phase 2): +20 to 0mV Refractory phase
- Longest phase of action potential due to slow Ca+ movement into cell and K+ out of cell to maintain voltage.
- Repolarisation (Phase 3): -90mV
- Simultaneous Ca+ & K+ movement out of cell reduces voltage until resting membrane potential is reached.
Page contributors:
 | Thanh Bui, AP60825 Event Medic, Emergency Medical Technician & Volunteer Development Officer
|
 | Andrew Moffat, AP16790 |
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.