
Emphysema is characterised by large permanently inflated alveolar air spaces due to the destruction of the alveolar walls and septae. The primary cause of emphysema is cigarette smoking and to a lesser extent other air pollutants. A genetic factor has also been identified as a contributor to early development of the condition in non-smokers. Below is an outline of the differing mechanisms in which the alveoli become damaged.
- Cigarette smoking and exposure to other air pollutants triggers an immune response by the body which amongst other things increases the amount of neutrophils (white blood cells) in the alveoli. Neutrophils play an essential role in the immune response however in this case they also have a damaging effect as they release protease, a destructive group of enzymes that begin protein catabolism. The most damaging of these enzymes is called elastase which is responsible for breaking down elastic fibres. What further compounds the problem and accelerates the damaging effects of the protease enzymes is that cigarette smoke and other air pollutants decrease the effect of alpha-1-antripsyin, a substance which usually fights and removes the protease enzymes. Therefore an imbalance is created with a large amount of protease enzymes being present in the alveoli which greatly contributes to the loss of proteins responsible for keeping the lungs elastic and also for destroying the tissue separating the alveoli from one another.
- Mucous and other secretions cannot be cleared from the airways as effectively due to cigarette smoke and other air pollutants temporarily disrupting the cilia (fine “hairs” which line the airways and clear fluids through a sweeping action). Long term exposure to cigarette smoke causes the cilia to disappear from the cells lining the airways and mucous and other secretions begin to build up. The accumulation of mucous is also accelerated as smoking and some other air pollutants cause mucous production to increase. Mucous is a good medium for bacteria and other organisms to proliferate and may lead to infection. Infection leads to the release of more neutrophils to the alveolar with some types releasing proteases. This leads to an even greater number of protease enzymes to be present and thus further contributing to the breakdown of the alveolar.
- In some individuals a genetic deficiency of alpha-1-antitrypsin can also contribute to the destruction of alveolar tissue. People with alpha-1-antitrypsin deficiency cannot fight the destructive effects of the protease enzymes once it is released in the lung causing alveolar destruction at an even greater rate (as described above in point one).
The damage to the alveoli and other changes to the lungs have many negative effects on lung function as described below:
Alveolar wall breakdown
The breakdown in the alveolar walls (as demonstrated in figure 2) will result in the following:
- Decrease in the surface area available for gas exchange
- Loss of pulmonary capillaries which leads to a decrease in perfusion and the diffusion of gasses
- The loss of elastic fibres causes a loss in elastic recoil on expiration
- Decreased support for structures within the lungs (such as the small bronchi) which may lead to collapse of the walls and obstruction of airflow during expiration.
- Pulmonary hypertension
Fibrosis and thickening of the bronchial walls
This occurs due to chronic irritation and frequent infections associated with smoking and the increased mucous production. The effects that this has on lung function are:
- Narrowed airways (figure 2)
- Weakened walls
- Interference with passive expiratory airflow
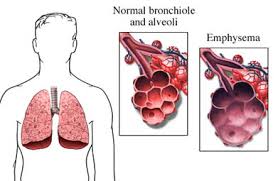
Figure 2: The breakdown of alveoli in emphysema and thickening of bronchial walls
Difficulty with expiration
Alveolar breakdown and thickening of the bronchial walls causes progressive difficulty with expiration. Over time this will lead to:
- Air trapping and increased residual volume
- Over inflation of the lungs
- Fixation of the ribs in an inspiratory position, and an increased anterior-posterior diameter of the thorax (barrel chest)
- Increased intrathoracic pressure
Advanced Emphysema and significant loss of tissue
If emphysema continues to progress (may happen rapidly if avoidance of respiratory irritants does not occur) the fore mentioned effects will gradually worsen leading to a significant loss of lung tissue. The following processes occur with these patients:
- Adjacent damaged alveoli combine forming very large air spaces called blebs or bullae (figure 2)
- The tissue and pleural membrane surrounding large blebs near the surface may rupture, resulting in pneumothorax
- Carbon dioxide (CO2) retention (Hypercapnia) becomes marked and hypoxic drive for inspiration develops as the patient’s respiratory control adapts to a chronic elevation of CO2 levels. (see drive to breath on page 6)
In the late stages pulmonary hypertension and cor pulmonale (enlargement of the right side of the heart) occurs due to pulmonary blood vessels being destroyed coupled with vasoconstriction caused by hypoxia. The increased pressure in pulmonary circulation puts a large strain on the right ventricle leading the patient to display signs of heart failure.
Page contributors:
 | Default Author St John WA |
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.