
Definition
Chronic obstructive pulmonary disease, or COPD, is a term used to describe a set of lung diseases that cause respiratory problems, by blocking airflow and making it hard to breathe. Diseases associated with COPD include some forms of bronchiectasis, chronic asthma, emphysema, and chronic bronchitis.
The effects of COPD are often well established and irreversible by the time a diagnosis is made however it can usually be managed effectively in most patients providing they modify their lifestyle and adhere to their prescribed medications. COPD is not an emergency presentation however when COPD sufferers contract respiratory infections exacerbation of the condition with sudden dyspnoea can occur due to their lung function being so compromised. Therefore it is essential for paramedics to have a good understanding of COPD as there are many patients living in the community who will require emergency care due to acute exacerbation of their illness. This document will describe the pathophysiology and explain the signs and symptoms of the common COPD conditions of emphysema, chronic bronchitis and bronchiectasis. It is however important to note that the diseases characteristics can overlap and share many common features.
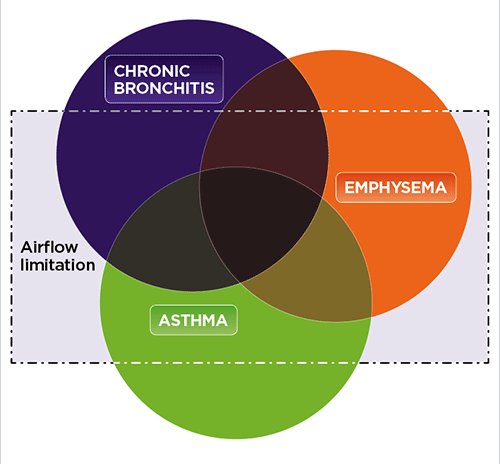
The two most common types of COPD include chronic bronchitis and emphysema. Both are characterized by damage to the lungs that prevent proper respiratory functioning. Main clinical features include shortness of breath, wheezing and a chronic phlegmy cough.
COPD is also known by the following names:
- COAD (Chronic Obstructive Airways Disease)
- COLD (Chronic Obstructive Lung Disease)
- CAL (Chronic Airways Limitation)
- CORD (Chronic Obstructive Respiratory Disease).
Key Terms:
- Emphysema
- Permanently enlarged/over-inflated alveolar due to the destruction of the alveolar walls.
- Chronic Bronchitis
- Hypersecretion of mucous and chronic productive cough for at least 3 months of the year for at least 2 consecutive years.
- Bronchiectasis
- Permanent distortion and dilation of bronchi and bronchioles.
- Ventilation/Perfusion (VQ) Ratio
- Used to measure the efficiency of alveoli gas exchange. VQ scans examine the ratio of air that reach the alveoli compared with the blood that reach the alveoli.
- V = ventilation; the air that reaches the alveoli
- Q = perfusion; the blood that reached the alveoli
- Normal alveolar ventilation= approx 4L/min
- Normal pulmonary capillary blood flow= approx 5L/min
- Normal V/Q ratio= 0.8
- Used to measure the efficiency of alveoli gas exchange. VQ scans examine the ratio of air that reach the alveoli compared with the blood that reach the alveoli.
Pathophysiology:
Emphysema:
- In patients with COPD, exposure to cigarette smoke leads to the destruction of alveolar walls and the permanent over inflation of alveolar air spaces.
- During exposure to cigarette smoke, neutrophils and macrophages (white blood cells) gather in alveoli.
- Excessive exposure to neutrophils and macrophages leads to a breakdown of elastic fibres in the alveolar, the thickening of bronchial walls and the loss of pulmonary tissue.
- Breakdown of elastic fibres leads to:
- Decrease recoil within the alveoli
- Air trapping
- Lung over inflation – barrel chest
- Decrease recoil within the alveoli
- Thickening of bronchial walls leads to:
- Narrowed airways
- Narrowed airways
- Loss of pulmonary tissue leads to:
- Decreased gas exchange
- VQ (ventilation/perfusion) mismatch
- Decreased gas exchange
Chronic Bronchitis:
- Inhaled irritants (smoke) cause increase in neutrophil presence, resulting in inflammation within the bronchial wall.
- Constant inflammation increases the size and number of goblet cells and mucous glands.
- This process leads to the reduction of cilia resulting in inability to clear mucous.
- Impaired ciliary function and increased mucous production lead narrowing airways.
Bronchiectasis:
- Often secondary to other respiratory disease or previous childhood chest infections.
- Recurrent airway infection and inflammation leads to deterioration in muscle and/or elastic fibres within bronchial walls.
- Widened bronchi allow mucous to pool.
- Stagnant mucous provides excellent medium for bacteria to develop.
VQ Mismatch:
Increased VQ ratio can develop from increased ventilation (i.e. increased PaO2) or decreased perfusion (i.e. decreased PaCO2); examples include:
- Pulmonary embolism
- Pulmonary hypertension
- Haemorrhage
- CPR
An example of increased VQ mismatch:
- Normal alveoli ventilation = 4L, with decreased perfusion (e.g. 2L) will produce increased ratio of 2.
This will show an increase in capnographic end-tidal CO2 (etCO2).
Decreased VQ ratio can develop from decreased ventilation (i.e. decrease PaO2) or increased perfusion (i.e. increased PaCO2); examples include:
- Airway obstruction- foreign body aspiration
- Chronic bronchitis
- Pneumonia
- Pulmonary fibrosis
An example of decreased VQ mismatch:
- Normal pulmonary blood flow = 5L, with decreased ventilation (e.e. 1L) will produce VQ mismatch ratio of 0.2
This will show a decrease in capnographic end-tidal CO2 (etCO2).
COPD and Carbon Dioxide Retaining
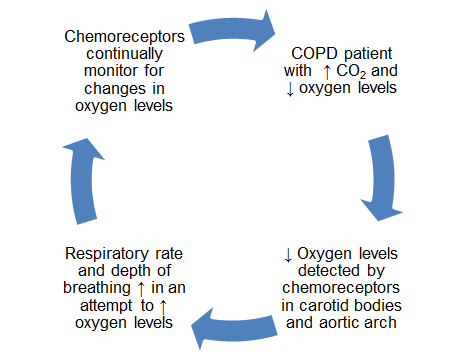
As previously described the disease process of COPD leads to high arterial levels of CO2. CO2 is able to cross the blood-brain barrier where it combines with water in the cerebrospinal fluid where it separates to form hydrogen ions and lowers pH levels. This triggers a reaction in the central chemoreceptors located near the medulla which are responsible for regulation. An increase in carbon dioxide levels leads to an increase in the depth and rate of respiration. Decreased levels of carbon dioxide will cause pH levels to rise and therefore a decrease in the depth and rate of respiration will occur. COPD leads to chronically high arterial levels of carbon dioxide and decreased levels of oxygen. Overtime this causes desensitisation of the central chemoreceptors. This causes a shift in the stimulus of ventilation to be managed by the peripheral chemoreceptors located in the carotid bodies and the aortic arch. These receptors are stimulated by oxygen levels rather than CO2. This means that when low levels of Oxygen are detected respiratory rate and depth of breathing will increase (Figure 5). When oxygen levels are high the opposite will occur. This is referred to as hypoxic drive.
A common misconception is that supplemental oxygen given to COPD patients will cause chemoreceptors to detect sufficient oxygen levels and not trigger the drive to breathe leading to respiratory failure. This is not the case in the majority of patients; only a small number of patients with COPD can become desensitised to abnormally high levels of carbon dioxide found in the bloodstream caused by poor lung function. Where this occurs, low oxygen levels, rather than high carbon dioxide levels, become the stimulus to breathe. More commonly what may happen is increased hypercapnia occurring over a period of time due to the introduction of supplemental oxygen. Due to this reasoning there is a mindset in some clinicians that administering supplemental oxygen to COPD patients will cause respiratory failure or a significant increase in hypercapnia. This belief frequently results in the reluctance of clinicians to administer oxygen to hypoxemic patients with COPD. As paramedics it is very important to remember that hypoxia can have permanent and irreversible effects to patients and in the acute setting has vastly more damaging affects than hypercapnia. Therefore in COPD patients with low oxygen saturations it is important to still provide supplemental oxygen aiming for saturations of 88-92%. Remember, hypoxia kills, hypercapnia happens!
Signs and Symptoms:
Emphysema:
- Dyspnoea (shortness of breath)
- Chronic non-productive cough
- Wheeze
- Difficulty exhaling
- Weakness on exertion
- Barrel chest
Chronic Bronchitis:
- Dyspnoea (shortness of breath)
- Constant productive cough
- Wheeze
- Chest pain, due to cough
- Peripheral Oedema
Bronchiectasis:
- Dyspnoea (shortness of breath)
- Chronic cough
- Up to 240ml of mucous production per day
- Foul breath
- Haemoptysis
- Frequent lung infection
Risk Factors & Comorbidites
- Current smoker (or inhalation of noxious gases/substances over period of time).
- Aged ≥ 50yo.
- Long standing airway disease, such as asthma
Risk factors such as smoking, age and obesity can complicate the association of COPD with certain comorbidities. The interaction between some medications can also add to this challenge. ie. administering bronchodilators may induce cardiac dysrhythmia. Administering β-Blockers may worsen lung function. However comorbidities such as HTN, cardiovascular disease and diabetes are so prevalent in patients with COPD that they must be considered during assessment.
Treatment
In the treatment of an acute exacerbation of COPD, oxygen should be administered. The hypoxic drive theory has made many paramedics overcautious of administering oxygen. Although during oxygenation respiratory rates can reduce in some patients with COPD, within 15 minutes, the respiratory rate typically returns to sufficient levels.
Patients with COPD optimise gas exchange due to hypoxic vasoconstriction. During excessive O2 administration, vasodilation occurs which moves blood to inadequately ventilated areas of the lungs. This results in reduced O2 absorption and increased CO2 retention.
Therefore "controlled or low dose supplemental oxygen" therapy should be utilised. Although over-oxygenation may have a detrimental effect, insufficient-oxygenation will be fatal.
The Haldane Effect
- If the pressure of oxygen in the blood is high, haemoglobin will release CO2 (normal in the lungs).
- If the pressure of oxygen in the blood is low, haemoglobin will bind to CO2 (normal in the tissue).
- During over oxygenation, the release of unbound CO2 will significantly increase.
- As the pressure of CO2 in the lungs will therefore be greater than O2 (which is abnormal due vasodilation), haemoglobin will bind to CO2 with greater affinity than O2 and subsequently reduce oxygenation.
Documentation:
Information Required (SAMPLE)
- Signs and symptoms (see above)
- Allergies
- Medication:
- Particularly if on home oxygen and at what flow rate (indicates patient is more likely to be CO2 retainer)
- Past medical history:
- Emphysema, chronic bronchitis, bronchiectasis, chronic asthma
- Normal SpO2 readings (usually between 88-92%)
- Smoker/ex-smoker
- Recent chest infections
- Last oral intake
- Events leading up to:
- e.g. chronic breathlessness, worsening over time, etc.
- Any recent signs of infection (fever, chills, productive cough)
Page contributors:
 | Default Author St John WA |
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.