
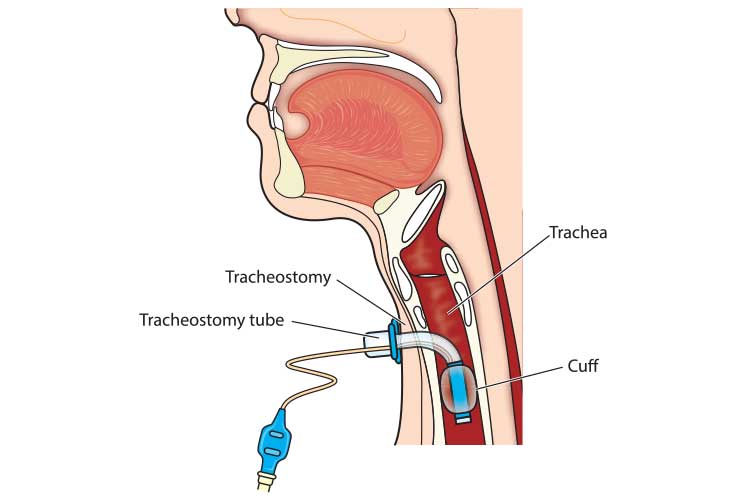
A tracheostomy is a surgical procedure that involves making an incision (stoma) into the trachea through the front of the neck. A tube is then inserted into the incision, creating an air passage that allows the patient to breathe directly through their trachea while avoiding their upper airway. This may be a temporary or permanent intervention (Healthdirect 2018; Mayo Clinic 2019). You may be called to assist a patient or caregiver with a tracheostomy in the pre-hospital arena; it is vital to ensure you care for a tracheostomy carefully and thoroughly, as an adverse event such as respiratory distress may develop if the tracheostomy is not managed properly.
Patient care and safety may be compromised if correct tracheostomy procedures are not followed. Suctioning performed improperly can cause complications such as hypoxia, atelectasis, bradycardia, trauma and infection. Airway impairment can be life threatening.
When dealing with tracheostomy tubes, ensure that Standard & Transmission-based Precautions are employed. Perform hand hygiene and put on personal protective equipment (PPE). Maintain the sterility of the catheter.
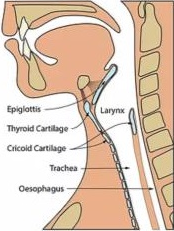
Normal airway
Laryngectomy
Tracheostomy
Background
There are a variety of tracheostomy tubes available with some or all of the following features, depending on what the patient requires:
- An inner cannula is a small tube inserted into the larger outer tube. It can be removed for cleaning while the outer tube stays in situ, helping to prevent mucus build-up.
- A cuff is a balloon on the outside of the tube, which inflates and creates an airtight seal against the airway walls. It prevents air from escaping through the nose and mouth and can also prevent the aspiration of saliva. Mechanically ventilated patients with tracheostomies require cuffs.
- An obturator/introducer attaches to the tracheostomy tube, creating a smooth, round tip. It is only used during the insertion of a tube to prevent damage to the trachea. It should be removed and discarded after tube insertion.
- Fenestrations are small holes on the upper surface of the tube that allow air and secretions to pass into the upper airways. Fenestrations help to facilitate speech, however, care should be taken to ensure they do not become blocked by downward-passing secretions.
- Sub-glottic suction ports facilitate suctioning above the cuff to prevent secretions from accumulating and going into the patient’s airway.
(NSW DoH 2015; Dawson 2014; Craig Hospital 2014; CCAM 2016)
Airway Profile
All children in Western Australia with a tracheostomy will have an Airway Profile. The Airway Profile will outline:
- Tracheostomy tube type (cuffed /uncuffed), size and the appropriate smaller size tube
- Suction depth
- Patient-specific airway information
- Ventilator settings, if applicable
- If patient has a speaking valve, whether it is drilled / undrilled and if used throughout the day
Complications
Tracheostomy airway impairment may occur due to:
- Partially blocked tube
- Completely blocked tube
- Accidental decannulation or dislodgement of the tube.
Emphasis is on early recognition of any change in the patient’s respiratory status and tube patency to avoid an emergency event. Late signs of impending respiratory collapse include cyanosis, bradycardia and apnoea – do not wait for these to develop before intervening.
Officers should familiarise themselves with the Tracheostomy / Laryngectomy Airway Emergencies Clinical Practice Guideline, and Suction - Tracheostomy Clinical Skill to manage these complications.
Management
If the patient is breathing on their own:
- Position & reassure
- Inform family
The patient is not breathing on their own:
- The tracheostomy tube is in place and patent:
- Commence respiratory support by connecting bag-valve mask to the tracheostomy tube and commence bagging. Be mindful of ventilation rate and tidal volume, being cautious not to hyperventilate or over-inflate.
- The tracheostomy tube is not in place:
- Request caregiver to re-insert tracheostomy tube.
- If successful, follow instructions above.
-
Unable to ventilate, follow instructions below.
- SJA personnel may assist, but are discouraged from performing this procedure independently (as this skill is deemed a competency).
- All children carry an emergency management kit equipped with a same size tracheostomy tube and a size smaller tracheostomy tube.
- Attempt to reinsert same size tracheostomy tube with lubricant prior to providing bag valve mask ventilation.
- If unable: size smaller tube with lubricant
- If caregiver unable to reinsert tracheostomy tube, provide bag valve mask ventilation per the instructions below.
- Dry the stoma area
- Cover stoma with an air tight dressing e.g. Tegaderm®
- Use bag valve mask (with appropriate sized face mask), covering the mouth and nose and commence ventilation as per clinical skill
- Apply gentle pressure over stoma, if required
- Position to optimise airway and breathing
- Use a bag valve mask (with neonatal mask) to cover the stoma and attempt to ventilate.
(Note: bag valve mask via nose/mouth are likely to be ineffective)
Suction should maximise removal of secretions while minimising tissue damage and hypoxia in order to maintain a patent airway and allow effective ventilation.
The routine suction depth will be recorded on the patient’s Airway Profile. Deep suctioning is not to be performed.
- If the patient is able to cough up their own secretions this should be encouraged.
- Suction can raise intracranial pressure and should be used with caution in patients with a head injury and conditions related to raised blood or intracranial pressure.
- The patients caregiver should be able to provide additional suction catheters if those provided are not suitable; they may also be able to provide a suction unit if there are incompatibilities with SJA carried equipment.
- Routine suction depth is 0.5cm beyond the tip of the tracheostomy tube. The suction depth on the Airway Profile already includes this 0.5cm.
| Tracheostomy tube size (mm) | 3.0 | 3.5 | 4.0 | 4.5 | 5.0 | 6.0 | 7.0 |
|---|---|---|---|---|---|---|---|
| Suction catheter size (Fr) | 6.0 | 7.0 | 8.0 | 8.0 | 10.0 | 12.0 | 12.0 |
Procedure
- Position the patient, allowing access to the tracheostomy tube
- The patient can remain in a wheelchair in a reclined position with shoulder roll
- A young patient may be placed in a semi-recumbent position exposing the tracheostomy tube
- An older patient may prefer to sit
- Attach the suction catheter to suction tubing, remove packaging and turn on the suction
- The LCSU4 suction unit has a pressure gauge and variable suction dial; set to between 80-120mmHg/10-16kpa by occluding the suction catheter and rotating the dial on the side of the unit until the LED indicators increase/decrease to the desired setting
- If you are not equipped with an LCSU4 unit (and are still using the ComWeld StatVac II unit in the Ferno Oxygen Bag), check with the parent/caregiver if they have a variable suction unit available.
- Note: Higher pressure may cause alveolar collapse, mucosal damage or catheter collapse, whilst inadequate suction pressure may not remove enough secretions resulting in increased number of catheter passes.

- Observe the patient during the procedure for signs of respiratory and cardiovascular instability and discomfort.
- If this occurs suction will need to be discontinued.
- Insert catheter into tracheostomy tube to the predetermined depth as specified on the patient’s Airway Profile.
- Protect the catheter tip from coming into contact with surfaces, hands and clothing – discard if contaminated and use a new catheter.
- If the catheter does not pass easily into the tracheostomy tube do not force, suspect a blocked or partially obstructed tube.
- The suction depth on the Airway Profile already includes the 0.5cm below the end of the tracheostomy tube.
- Suction should be applied on withdrawal of the suction catheter to minimise mucosal damage in the respiratory tract.
- It is not necessary to rotate the catheter as the multiple eyelet catheters will remove secretions effectively.
- Assess the patient and the effectiveness of secretion clearance.
- Repeat the procedure if necessary.
- Do not contaminate the catheter tip between passes.
- If the suction catheter is not contaminated between suction passes it can be reused for multiple passes then discarded.
- Re-assess the patient, in terms of respiratory effort, adventitious lung sounds & colour
- Dispose of suction catheter. Suction tap water through the suction tubing to clear it of secretions.
- Discuss with the caregiver reattaching any external devices (e.g. Swedish nose, speaking valve) which were removed prior to starting procedure; these may stay disconnected in case the patient requires suctioning during ambulance transport.
References
- Tracheostomy Management.
- Royal Children’s Hospital. Tracheostomy Management. In: Clinical Nursing Guidelines, editor. Melbourne Australia: The Royal Children's Hospital Melbourne; 2018.
- Perth Children's Hospital. Tracheostomy Management Guideline. In: Clinical Practice Manual, editor. Perth: Child and Adolescent Health Services; 2018.
- Perth Children's Hospital. Tracheostomy Resuscitation Procedure. Clinical Practice Manual. Perth: Child and Adolescent Health Services; 2017.4.
- Credland N. How to suction via a tracheostomy. Nurs Stand. 2016;30(28):36-8
Page contributors:
 | Deane Coxall, AP14227 Clinical Services |
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.