
Typical Behaviours of impulses includes;
- Bradycardia (Slow)
- Usually from dysfunctional automaticity of pacemakers or impulse block resulting in slower impulse
- Tachycardia (Fast)
- Resulted from impulse spreading out from atria (Supraventricular) or ventricle (Ventricular) resulting in rapid/faster impulse.
For treating heart failure and irregular heartbeat like AF – The drug enhances ventricular contractility but lowers heart rate by making more calcium available and increasing vagus nerve activity (cause diminishes SA node automaticity).
- ST depression with curved appearance will occur
- T-wave amplitude diminishes (can appear biphasic) or inverted wave
- U-wave slightly increase in amplitude
- QTc interval shortened at therapeutic doses
For treatment of ventricular tachyarrhythmias or AF
- Prolonged QRS
- ST depressions may develop
- T-wave may diminish in amplitude
- QT & QTc interval may prolong
- May provoke ventricular arrythmias
For treatment of ventricular tachyarrhythmias or symptomatic paroxysmal supraventricular tachyarrhythmias.
- Prolonged QRS
- QT & QTc interval may prolong
Antiarrhythmic drug for serious SVT or VT, and WPW syndrome & AF.
- Prolonged QRS
- Wider T-wave
- Obvious U-wave
- QT & QTc interval may prolong
- Sinus bradycardia &/or torsade de pointes may show
Acute treatment of SVT & VT or controlling AF after return to sinus rhythm.
- PR interval prolonged
- QT & QTc interval may prolong
Role to reduce effect of catecholamines on the heart resulted from low heart rate, &/or decrease conductivity – aim to block the effect of adrenaline.
The SA node decreases in automaticity (sinus rate decrease)
- PR interval prolonged
- QT & QTc may be shortened
- Slower heart rate seen
Prevention of calcium from entering the heart cells and arteries decreasing the muscle action – This therefore, cause muscle relaxation – Less forceful contractions, vasodilation etc.
- PR interval prolonged
- QT & QTc may be shortened
Increased (hypernatremia) or decreased (hyponatremia) sodium levels do not affect the ECG as sodium is more related to fluid volume control.
Caused by hyperthyroidism or malignancies in most causes – other imbalances or diseases can cause this condition;
- Shortened QT interval (longer QRS duration)
- Bradycardia may occur
Potential complications can occur;
- Increased QRS amplitude
- Diminished T-wave amplitude
- STE in V1-V2
- All degrees of AV block
- Osborn-like waves
Caused by issues relating to the pancreas, sepsis, alkalosis or GIT issues.
- Lengthened QT interval (short QRS duration)
- Torsade De Pointes can occur
Potential complications can occur;
- AV block
- Sinus bradycardia
- SA block
- VF
Hypermagnesemia is rare but can cause AV and intraventricular conduction disturbance which can result in asystole or third-degree AV block.
Hypomagnesemia can turn into effects of digoxin and show SVT or VT.
High levels of potassium resulting in decrease impulse transmission to the whole heart – Caused by many medical factors and diseases.
Mild (> 6mmol)
- Pointed T-waves (tall & narrow top)
- LVH patients can show secondary T-wave inversion (V5-V6, aVL & Lead I)
Moderate
- Like mild symptoms but more pronounced
- Wider P-wave (amplitude decrease)
- PR prolonged
- WPW syndrome patient loses delta-wave
- STE in V1-V3
Severe (> 7.5mmol)
- Like mild & moderate but more pronounced
- Wide QRS
- QRS may fuse with T-wave (forms sine wave)
- VF may occur after sine wave is formed
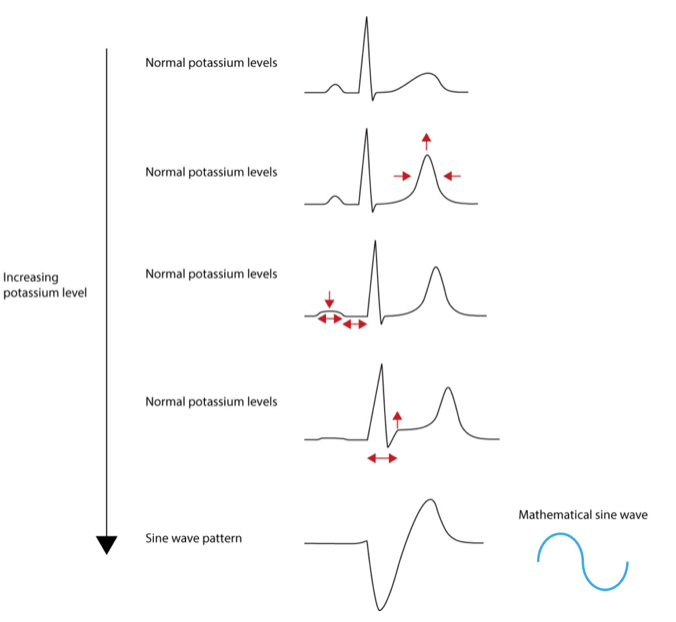
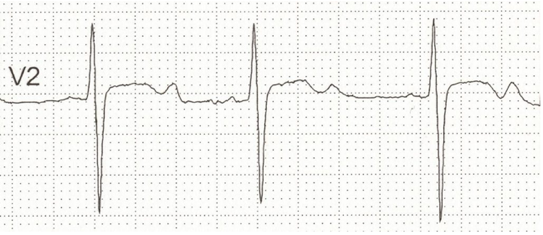
When levels are < 3mmol from fluid loss, malnutrition, medical/injury or alcohol use – Can be caused by medications such as steroids or diuretics & insulin.
- Wider T-wave (lower amplitude)
- ST depression can occur with T-wave inversion
- P-wave amplitude & duration increase (increase PR interval)
- U-wave emerge (Usually V2-V3)
- U-wave can be larger than T-wave in worse case
Page contributors:
 | Thanh Bui, AP60825 Event Medic, Emergency Medical Technician & Volunteer Development Officer
|
 | Andrew Moffat, AP16790 |
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.