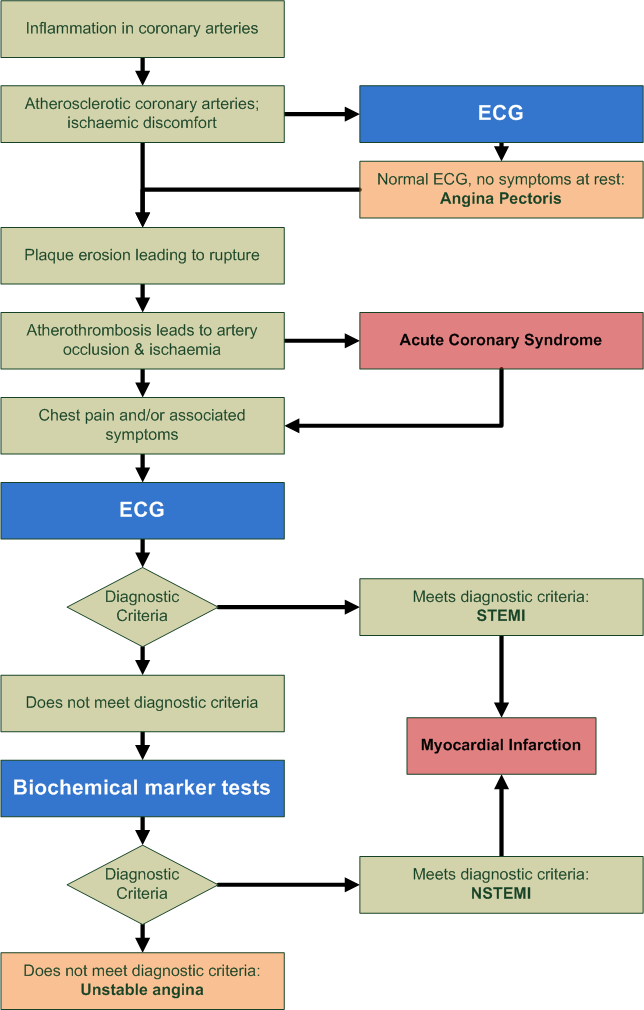
Acute Coronary Syndrome (ACS) is a coronary artery disease causing many changes in the ECG such as ST elevation & angina.
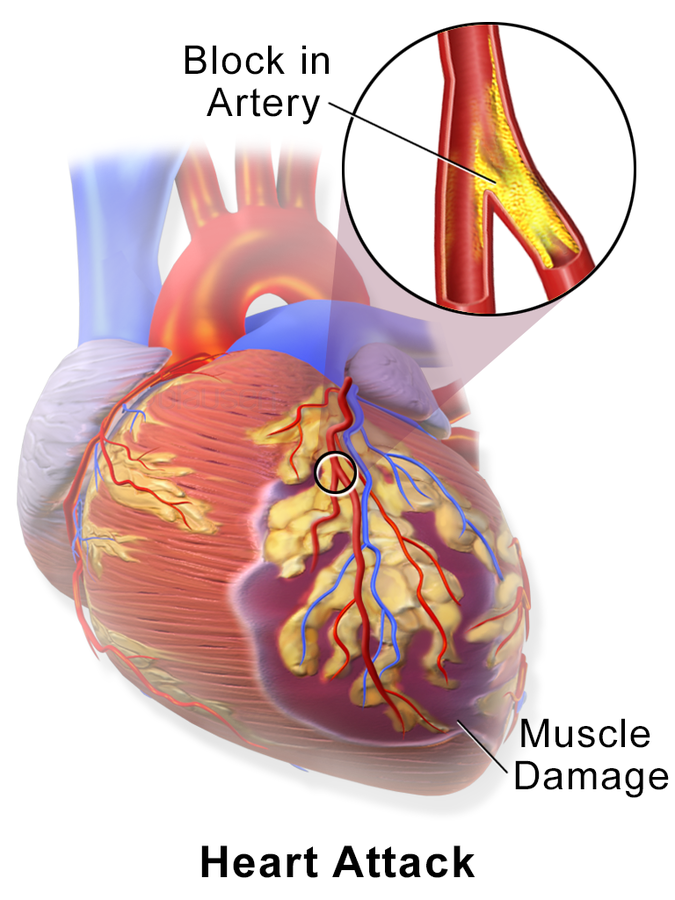
- Ischemia: Interruption of coronary heart supply temporarily, usually 70% blocked or more where cardiac oxygen demand is higher than supply. This results in cardiac chest pain symptoms as the heart cannot get electrolytes nor remove
waste which impairs repolarisation or relaxation
- Hence T-wave changes
- ST depression can occur with prolonged ischemia
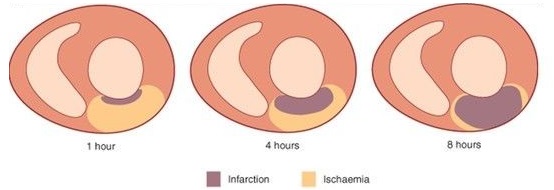
- Injury: Complete occlusion (blockage) of the coronary vessel resulting in spasms or rupture which injure the surrounding muscles. This is an acute phase for acute myocardial infarction (AMI). This phase only injures muscles, it has not died or necrotic yet – The vessel can be reopened and halt AMI to prevent further damage.
- Infarction: Prolonged interruption resulting in cardiac muscle death / necrosis. ST elevation can form acutely as it cannot lie normally on the isoelectric line normally.
- Q-wave develop (wider > 0.04s) in multiple leads and more than ¼ R-wave’s height.
- ST elevation is significant if > 1mm high in limb lead & > 2mm in chest leads in same group
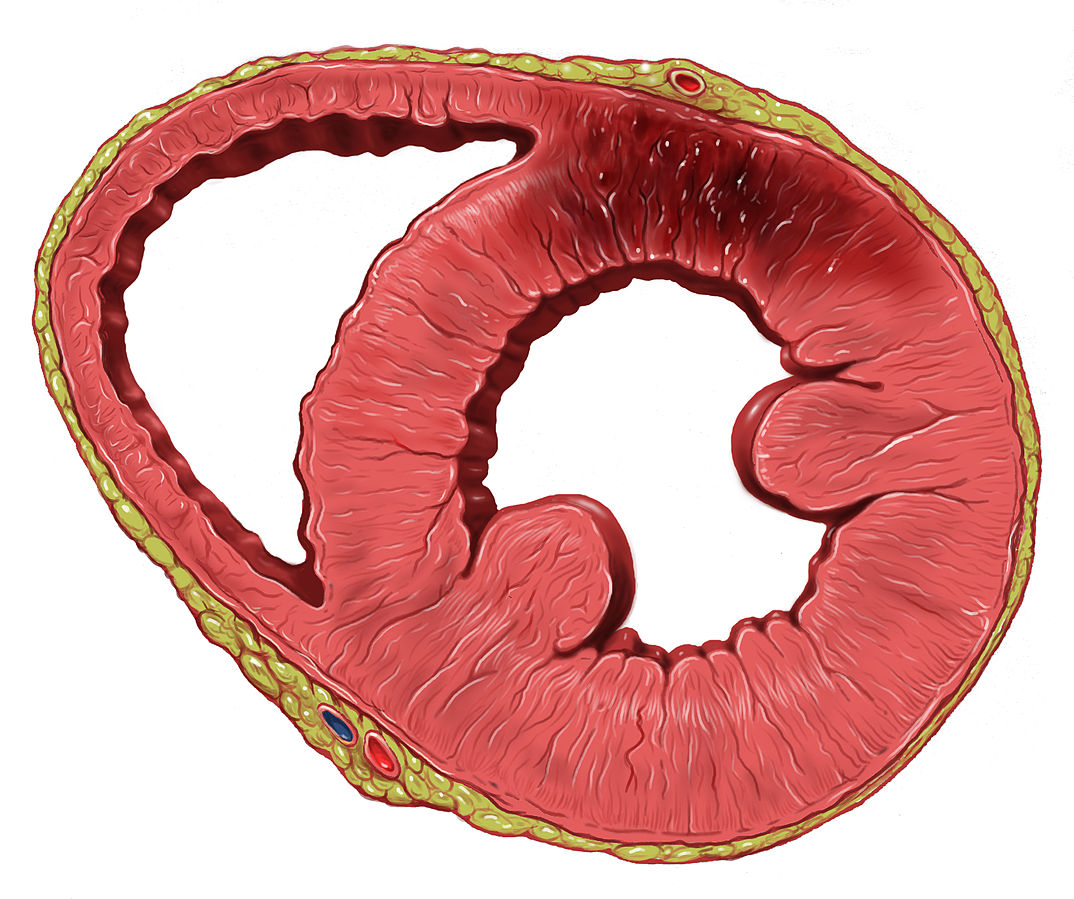
Ischemia can be transmural (entire wall thickness) &/or subendocardial (only subendocardium impacted).
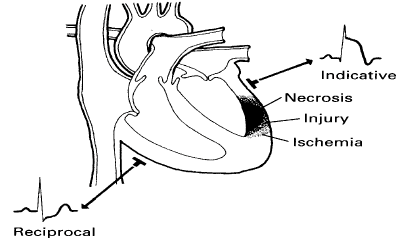
Reflection of ischemic area if it is shown in two (2) or more leads of the same anatomical lead group such as V1 & V2 / V5 & V6 / aVF & Lead III etc. Changes in one (1) lead only is not significant and is termed ‘involvement.’
For example - ST elevation in V1-V5 would be called “anterior AMI with lateral involvement”
Refer to ST depression present in other regions of the heart whilst there is ST elevation – This reflects on the view of the AMI from opposite sides and not clinically significant
- ST depression with ST elevation present = Reciprocal
- ST depression by itself = Prolonged ischemia / injury
| Lead | Lead I | aVR | V1 | V4 |
|---|---|---|---|---|
| Region | High Lateral | Septal | Anterior | |
| Reciprocal changes | II, III, aVF | |||
| Artery | Circumflex | Left Anterior Descending | Left Anterior Descending | |
| Lead | Lead II | aVL | V2 | V5 |
| Region | Inferior | High Lateral | Septal | Lateral |
| Reciprocal changes | I, aVL | II, III, aVF | II, III, aVF | |
| Artery | Right Coronary | Circumflex | Left Anterior Descending | Circumflex |
| Lead | Lead III | aVF | V3 | V6 |
| Region | Inferior | Inferior | Anterior | Lateral |
| Reciprocal changes | I, aVL | I, aVL | II, III, aVF | |
| Artery | Right Coronary | Right Coronary | Left Anterior Descending | Circumflex |
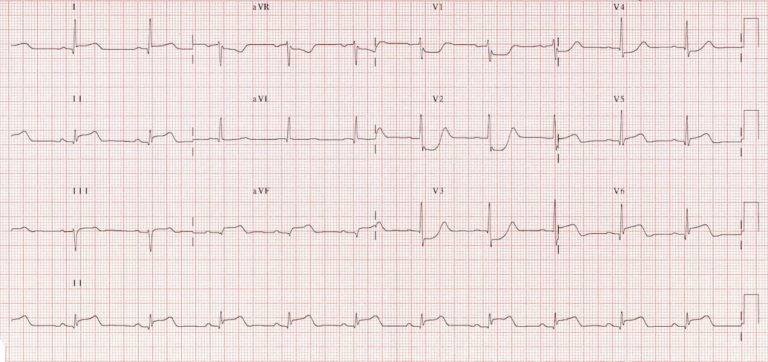
Beware of the 'normal ECG' on arrival; run multiple sequential ECGs, which may show progressive changes as the disease state continues.
For ACS symptoms that are not STEMI where an artery is partially blocked therefore there is still circulation therefore oxygen can reach the endocardium (but not the sub-endocardium).
ECG features include ST depression with T-wave changes (flat waves or inverted) – These ST-depression may not reflect ischemic area. Pathological Q-waves are not developed (hence infarction is usually small unless subendocardium infarction).
T-wave inversions with ST depressions indicates acute/ongoing ischemia where isolated T-wave inversion indicates post-ischemia after the ischemia episode.
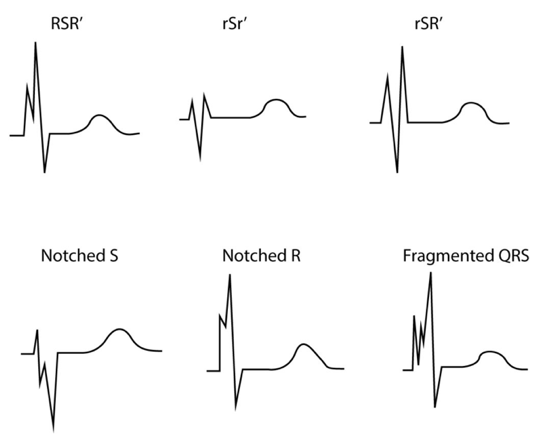
A fragmented QRS complex can be seen during or after infarction; in bundle branch blocks, >2 notches can be seen in in R-wave or S-wave.
- QRS complex with > 1 R-wave and/or
- Notch in descending limb of R-wave and/or
- Notch in descending limb of S-wave
QTc interval may also be prolonged, shortened or unchanged in ischemia
Q-wave behaviours includes being wider and deeper usually in transmural or inferior STEMI with diminishing waves overtime.
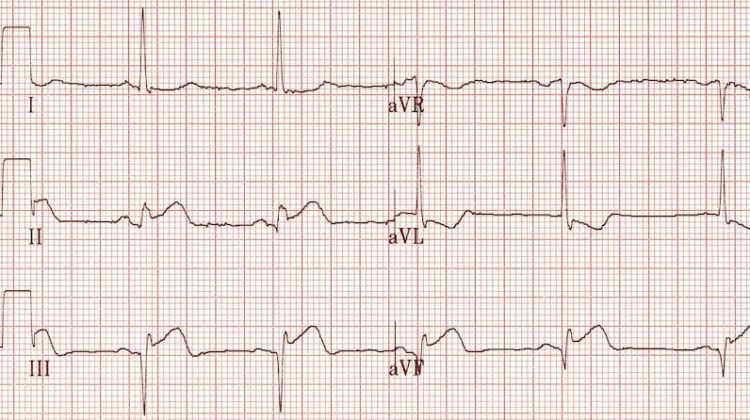
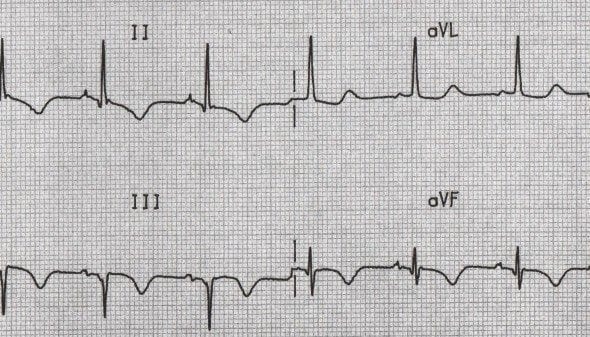
Inferior Q waves (II, III, aVF) with ST elevation due to acute MI
The R-wave has a reduced amplitude with an abnormal R-wave progression overtime – more specifically being lower than the pathological Q-waves – However, acute transmural ischemia may show increase in R-wave amplitude due to delayed depolarisation in the ischemic area.
Works with T-wave as they correlate to Phase 2 & 3 of electrical activity which is repolarisation. Changes depend on localisation, extension and time of ischemia (ie. It differs in later phases)
- ST segment may be elevated or depressed (in relation to PR segment)
- T-wave may lose (flat) increase amplitude (hyperacute), become negative (inversion)
- 1. Isolated T-wave inversions occur after ischemic episode (same as flat T-wave)
- 2. Hyperacute T-wave indicate isolated sign for SMI – Seen as broad and high
New U-waves (without bradycardia) may indicate ischemia – If U-waves are present in previous ECG recordings, then the amplitude must increase to suggest ischemia. Changes to U-wave are accompanied by ischemic ST-T changes in NSTEMI & STEMI - Inverted U-waves are typical signs of ischemia.
- ST Depressions
- Either horizontal or down sloping segment with potential abrupt transition from ST to T wave – This can occur in STEMI or NSTEMI.
- ST Elevation
- Can present in many forms, however concaved ST elevation are less likely from ischemia; can have differential diagnosis besides STEMI.
| Transmural Ischemia (Full thickness) | Effects seen |
|---|---|
Vector directed from endocardium to epicardium
|
|
| Subendocardial Ischemia (Partial thickness) | Effects seen |
|---|---|
Vector directed from endocardium to epicardium
|
|
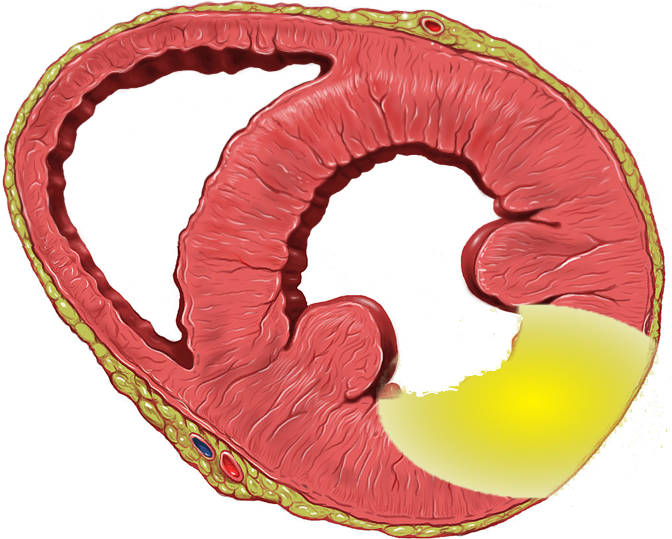
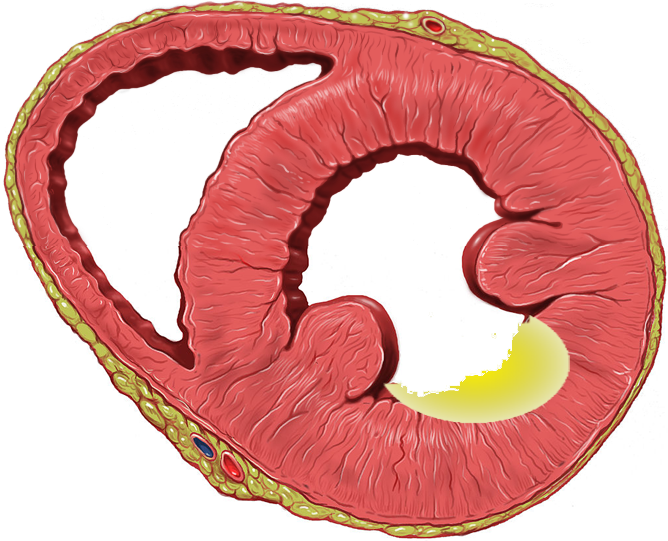
Transmural ischemia in posterolateral portion of left ventricles AND/OR right ventricles usually don’t show up on the ECG – These regions may have simultaneous ischemia at one time
Masked by the ECG – however leads V1-V3 (maybe V4) can detect injury currents as ST depressions (mirroring ST elevations) with positive T-wave in V1-V3 (mirrors T-wave inversion) as well as larger R-waves as reciprocal to posterolateral Q-waves.
It is recommended V4-V6 becomes V7-V9 by placing electrodes on the back.
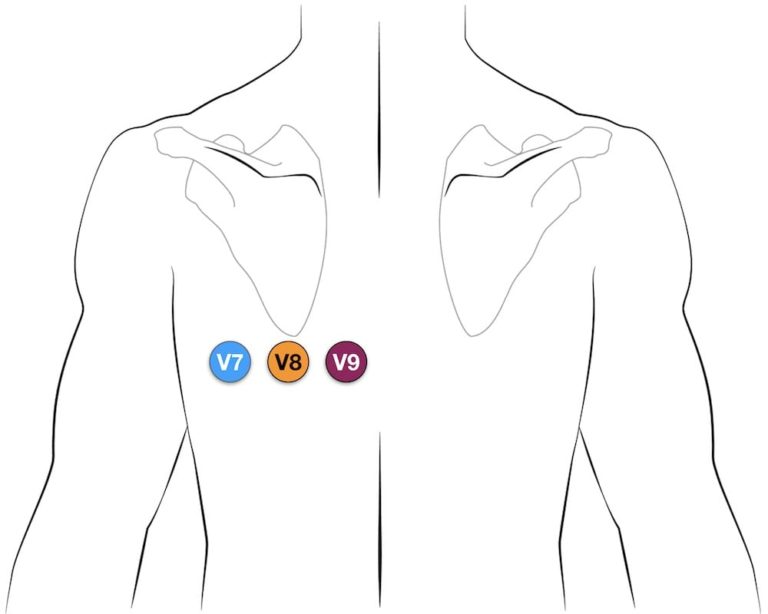
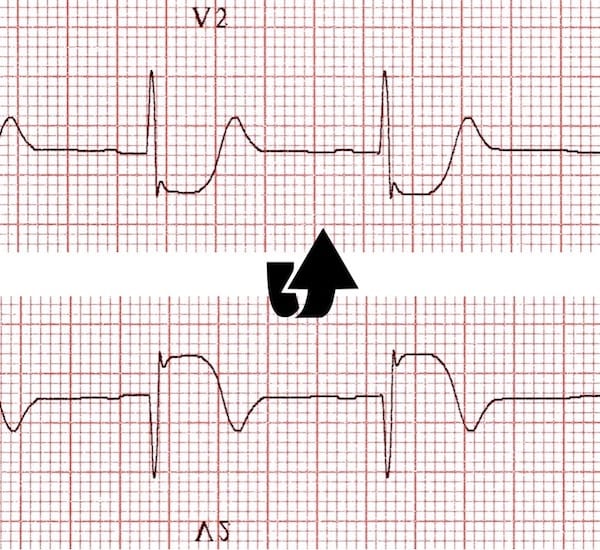
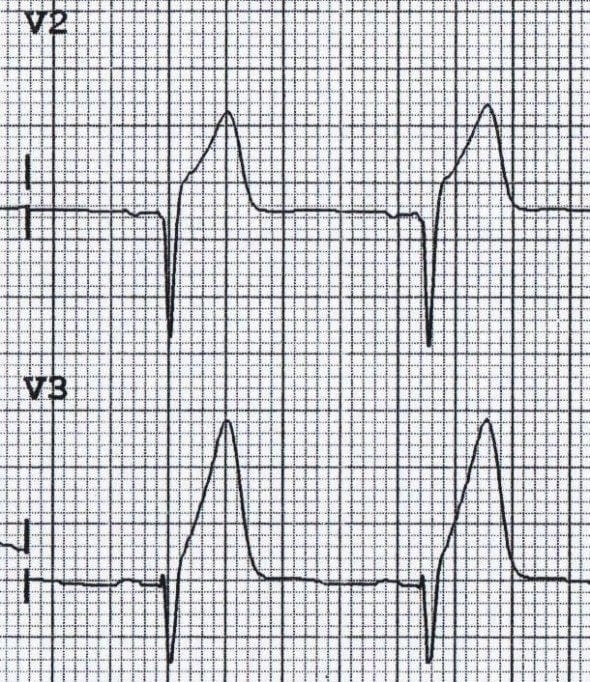
This picture illustrates the reciprocal relationship between the ECG changes seen in STEMI and those seen with posterior infarction. The previous image (depicting posterior infarction in V2) has been inverted. See how the ECG now resembles a typical STEMI!
- V1-V3 has ST depression & positive T-waves
- V1-V3 has larger R-waves
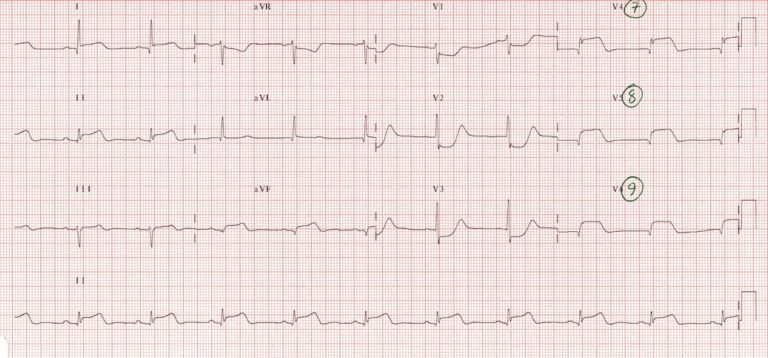
Rare blockage, however, V1-V2 can assist in determining STEMI in the right ventricles – the elevation are short duration and rarely persist after six hours, the ST elevations can be accurately recorded using right-sided ECG placement in V3R & V4R.
- ST elevation in V1 & V2, but elevation is higher in V1 than V2
- Most cases, ST elevation in Lead I, II, & aVF as it also sees the RCA.
Multiple ECGs must be taken to identify any ST-T changes as it can be missed due to the limited time the ECG captures the activity – This is bound to happen if ischemia occurs; furthermore, an ECG must be compared where ST-T changes suggest ongoing AMI.
A patient complaining of cardiac-related symptoms, chest region, or breathing difficulties should warrant further history collection and examination, including an ECG to rule out STEMI / NSTEMI.
| NSTEMI Signs | STEMI Signs |
|---|---|
|
|
Occur days or weeks after event (longer if infarction occur) – ST-T changes normalise with the permanent changes usually relate to the QRS complex (mostly Q-waves).
| Infarcted Artery | ECG Features |
|---|---|
| Inferior Wall | STE in Lead II, III, & aVF (STE highest in Lead III) with reciprocal ST depression aVL & Lead I |
| Inferior & Posterior (Inferobasal) | STE in Lead II, III, aVF & V7-V9; with reciprocal ST depression V1-V3, aVL, & Lead I – V1 to V3 can show high R-waves and positive T-waves |
| Inferior & right ventricle | STE in V3R to V6R with potential for STE in V1 & V2 (STE highest in V1) |
| Infarcted Artery | ECG Features |
|---|---|
| Proximal LAD | STE in V1-V4, aVL & Lead I with reciprocal ST depression in Lead II, III, aVF, -aVR, & V5-V6. |
| Distal LAD | STE in V2-V6 |
| Infarcted Artery | ECG Features |
|---|---|
| Posterior LCx | STE in V7-V9 with reciprocal ST depression in V1-V3 with high R-waves & positive T-wave in same leads. |
| Inferoposterior LCx | STE in Lead II, III, aVF (occasion in aVL, Lead I); just like inferior blockage |
| Main LCA | STE in most ECG leads due to large wall. |
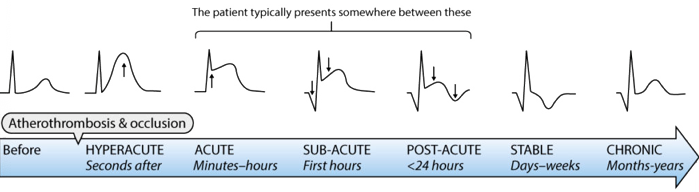
Identified by Q-waves & ST elevation (STE) as a reference
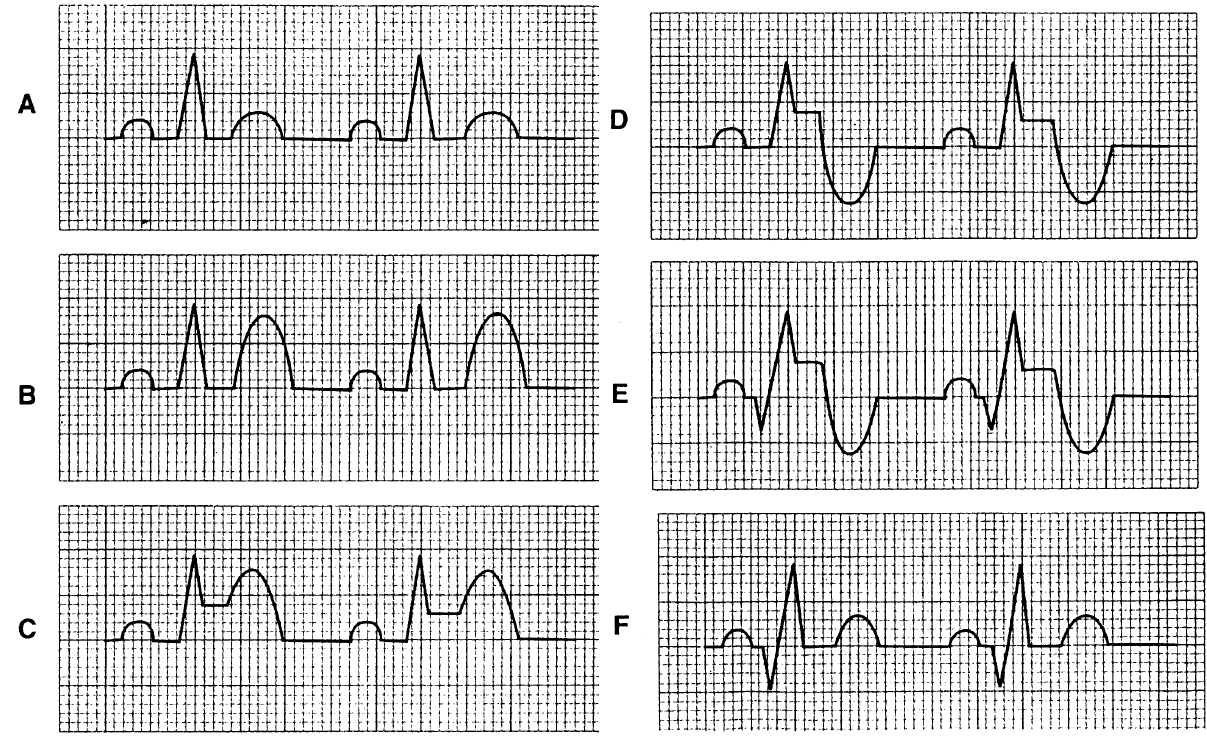
- ST Elevation in a region but NO Q-waves = Acute infarction Figure C & D
- Due to muscle not yet died – important as this indicate the vessel can be reopened and re-perfused.
- ST Elevation in a region WITH Q-waves = Infarction is > 2hrs ago Figure E
- Q-wave build from 2 to 4 hours after blockage, STE with Q-waves can indicate damage has been done but is still acute – Some cardiac muscle can be saved by doctors.
- No ST Elevation WITH pathological Q-waves = Old infarction Figure F
- ST segments return to baseline and T-wave can be inverted after an AMI has evolved. Furthermore, the T-wave can be upright along with no STE. Pathological Q-waves occur if the AMI is large (usually wide & deep wave).
Page contributors:
 | Thanh Bui, AP60825 Event Medic, Emergency Medical Technician & Volunteer Development Officer
|
 | Andrew Moffat, AP16790 |
Clinical Resources Website
St John Ambulance Western Australia Ltd (ABN 55 028 468 715) (St John WA) operates ambulance and other pre-hospital clinical services. St John WA’s Clinical Resources, including its Clinical Practice Guidelines (Clinical Resources), are intended for use by credentialed St John WA staff and volunteers when providing clinical care to patients for or on behalf of St John WA, within the St John WA Clinical Governance Framework, and only to the extent of the clinician’s authority to practice.
Other users – Terms of Use
The content of the St John WA Clinical Resources is provided for information purposes only and is not intended to serve as health, medical or treatment advice. Any user of this website agrees to be bound by these Terms of Use in their use of the Clinical Resources.
St John WA does not represent or warrant (whether express, implied, statutory, or otherwise) that the content of the Clinical Resources is accurate, reliable, up-to-date, complete or that the information contained is suitable for your needs or for any particular purpose. You are responsible for assessing whether the information is accurate, reliable, up-to-date, authentic, relevant, or complete and where appropriate, seek independent professional advice.
St John WA expressly prohibits use of these Clinical Resources to guide clinical care of patients by organisations external to St John WA, except where these organisations have been directly engaged by St John WA to provide services. Any use of the Clinical Resources, with St John WA approval, must attribute St John WA as the creator of the Clinical Resources and include the copyright notice and (where reasonably practicable) provide a URL/hyperlink to the St John WA Clinical Resources website.
No permission or licence is granted to reproduce, make commercial use of, adapt, modify or create derivative works from these Clinical Resources. For permissions beyond the scope of these Terms of Use, including a commercial licence, please contact medservices@stjohnambulance.com.au
Where links are provided to resources on external websites, St John WA:
- Gives no assurances about the quality, accuracy or relevance of material on any linked site;
- Accepts no legal responsibility regarding the accuracy and reliability of external material; and
- Does not endorse any material, associated organisation, product or service on other sites.
Your use of any external website is governed by the terms of that website, including any authorisation, requirement or licence for use of the material on that website.
To the maximum extent permitted by law, St John WA excludes liability (including liability in negligence) for any direct, special, indirect, incidental, consequential, punitive, exemplary or other loss, cost, damage or expense arising out of, or in connection with, use or reliance on the Clinical Resources (including without limitation any interference with or damage to a user’s computer, device, software or data occurring in connection with such use).
Cookies
Please read this cookie policy carefully before using Clinical Resources from St John WA.
The cookies used on this site are small and completely anonymous pieces of information and are stored on your computer or mobile device. The data that the cookies contain identify your user preferences (such as your preferred text size, scope / skill level preference and Colour Assist mode, among other user settings) so that they can be recalled the next time that you visit a page within Clinical Resources. These cookies are necessary to offer you the best and most efficient possible experience when accessing and navigating through our website and using its features. These cookies do not collect or send analytical information back to St John WA.
Clinical Resources does integrate with Google Analytics and any cookies associated with this service enable us (and third-party services) to collect aggregated data for statistical purposes on how our visitors use this website. These cookies do not contain personal information such as names and email addresses and are used to help us improve your user experience of the website.
If you want to restrict or block the cookies that are set by our website, you can do so through your browser setting. Alternatively, you can visit www.internetcookies.com, which contains comprehensive information on how to do this on a wide variety of browsers and devices. You will find general information about cookies and details on how to delete cookies from your device. If you have any questions about this policy or our use of cookies, please contact us.